A mother whose daughter was unexpectedly stillborn has detailed a series of hospital failings that left her watching police put her baby in a Styrofoam box and then being forced to identify the body at a mortuary.
Naomi Bowden, 41, cried as she told the NSW Birth Trauma Inquiry of her pain when detectives left her living room with her daughter Bella in a cooler.
No one explained how their daughter went from “fine” to dead in two hours, and no one explained that because she was on suicide watch, she was kept in the maternity ward all night and listened to nearby women give birth to healthy babies. .
Mrs Bowden’s suffering continued at a follow-up appointment six weeks later, when staff, who had not read her file, asked: “Where is your baby?”
Her story was just one of 4,000 submissions submitted to the inquiry, most of which came from women who experienced traumatic births in hospital.
Last week, a committee chairing the inquiry found these experiences “unacceptable, distressing and avoidable”, and its final report contained 43 recommendations for the NSW Health Minister to consider.
Naomi Bowden had a stillborn daughter in 2009 and says the way she was treated in hospital was traumatizing

Pictured: Naomi Bowden giving evidence at the September inquest.
At her presentation last September, Ms Bowden said she was medicated for depression throughout the pregnancy, but that it was otherwise a “textbook” pregnancy.
On the morning of November 4, 2009, she began experiencing contractions and went to Wollongong Hospital with her husband, Clint.
She felt calm and relaxed and gave the consultant midwife a copy of her birth plan which she had drawn up during an appointment with the hospital’s head of midwifery.
By 7 p.m., his blood pressure had skyrocketed, so hospital staff monitored the baby’s heartbeat using cardiotocography, assuring him that the baby was “fine.”
“The next minute I knew the registrar had entered the room to investigate further,” he said.
“He told me he needed to check the baby and wanted to do a ROT.”
ROT stands for “right occipital transverse”, which means Bella was looking towards the right side of her pelvis, rather than looking back as she should have been, but the registrar did not explain that to Ms Bowden.
When he agreed to the procedure, he didn’t realize it involved him inserting his hand to physically turn the baby’s head, or that it would be “one of the most painful experiences I’ve ever gone through.”
Hospital staff continued to monitor Bella’s heartbeat, but they sensed that labor was not progressing and said they would have to use forceps or a vacuum to get her out.
“I couldn’t push this baby out and it felt like I was sucking him back in after my contractions,” Ms Bowden said.
“They didn’t explain anything to me in detail and as far as I know, the baby’s heartbeat was fine.”
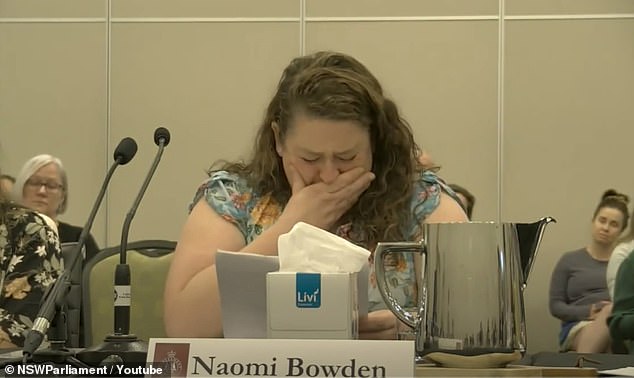
Naomi Bowden collapsed when giving evidence at the inquest last year (pictured)
Bella was born at 8:45 p.m. and the staff helped her husband cut the umbilical cord, but noticed that it wasn’t coiled like it should have been: it looked flat, like it had been crushed.
‘Could Bella’s rotation have compressed her cord? These are answers we never got,” her presentation read.
The situation then went from chaotic to horrifying.
Initially, hospital staff did not notice that Bella was not crying or moving when they handed her over to Mrs. Bowden; she was white, limp and unresponsive.
Suddenly, the staff took Bella away and the hospital staff began resuscitating her in the bed next to Mrs. Bowden.
“They rushed her out of the room with the doctors flying to her side and they left me to deliver the placenta,” she said.
‘The nurse told me to get in the shower because I was most likely going to go to the NICU unit or be flown to Sydney.’
By the time Mrs. Bowden came out of the shower, Bella was dead.
‘I fell to the ground broken, my husband fell to the ground and sobbed. What just happened? ‘How did this happen?’ she asked.
They were escorted to the NICU where they were greeted by a nurse who was “loud, abrupt, rude and disrespectful” and did not seem to know why the couple was there.
When he was finally able to see and hug Bella, he said it was horrible because she still had tubes coming out of her mouth.
The pediatrician didn’t contact the registrar and didn’t sign the death certificate, which meant the coroner was called and told Bella’s death was “unexplained.”
“We were told the police were coming to take Bella’s body to the coroner’s office in Sydney for an autopsy and we basically had nothing to say,” he recalled.
“It was distressing to have the police officers take her baby away from her and put him in a cooler.
“We had to identify to the police the body of our baby that I just gave birth to.”
No one at the hospital comforted her, tried to explain Bella’s death to her or helped her understand the situation, she said.
Weeks later, just before her six-week postnatal appointment, Ms Bowden was sent a stack of PDF files with a note on the front that said: “FYI, I haven’t read them yet, so I can’t give him his opinion.”
During the meeting, the consultant midwife discussed the documents and explained that they said the antidepressants Ms Bowden was taking could cause oxygen deprivation for babies.
“She was implying that that’s what happened to Bella and that’s why she died,” Mrs Bowden said.
‘We left that meeting unable to function…Due to my mental health and the medication I require, I compromised the health and well-being of my baby.’
Two years later, in 2011, they received the results of Bella’s autopsy and discovered that the midwife was wrong.
The baby did not die as a result of the medication, the situation was as Mrs Bowden had thought: it had suffocated as a result of prolonged labour.
A complaint was made to the Health Care Complaints Commission, but there was no formal investigation.
“I feel like it’s very unfair because if so many things were treated differently, I would have been a different person,” she said.
“It has affected my overall health, even to this day.”
Health Minister Ryan Park said the report was “sobering”, and now has three months to respond to the committee’s 43 recommendations.

