Mindfulness has been touted as a solution for everything from anxiety to depression, but according to new research, it could also help with chronic pain.
Veterans who took mindfulness classes for a year were able to cope with their pain better than veterans who only received traditional chronic pain treatments, such as painkillers and therapy.
This meditative practice, which has become increasingly popular in recent years, involves deep breathing and focusing on the moment, asking participants to let thoughts and emotions arise naturally without acting on them.
“Mindfulness-based interventions (MBIs) can improve chronic pain and comorbid conditions such as post-traumatic stress disorder (PTSD), sleep disorders, depression, and substance abuse, and are now recommended as first-line treatment,” wrote study author Dr. Diana Burgess, a social psychologist at the VA Health Care System.
Mindfulness may help people cope with chronic pain and associated problems such as depression, post-traumatic stress disorder and fatigue, according to the study.
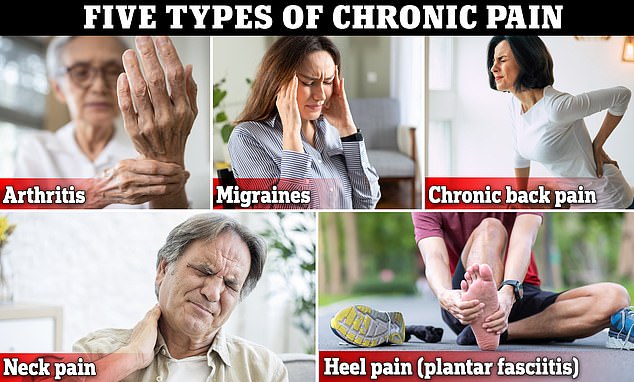
Chronic pain is estimated to have affected an estimated 51 million American adults in 2021. According to the Centers for Disease Control and Preventionand is defined as continuous pain lasting more than three months.
It has been linked to dementia, increased risk of suicide, and substance abuse.
Veterans are more likely than the average adult to suffer from this disease.
Since chronic pain can be caused by almost any part of the body, treatment varies.
It sometimes includes physical therapy, psychological therapy and medication. The medications used can range from paracetamol to antidepressants and opioids.
Researchers often look for better ways to tackle this widespread and difficult-to-treat disease. The new study, which Published in JAMA Internal Medicinesought to see if low-cost mindfulness programs could help people cope with pain.
The 694 participants were divided into three groups. The first group received traditional pain care, the second group had eight 90-minute group mindfulness classes, and the third group had eight self-directed mindfulness classes.
These classes included videos and workbooks explaining the concept of mindfulness and encouraging participants to use it to manage pain and everyday emotions. Group classes also included discussions.
After one year, the groups taking mindfulness classes had less severe pain, less anxiety, fatigue, depression and PTSD symptoms, as well as greater physical function than the group taking traditional therapy.
The mindfulness groups reported a 30 to 50 percent improvement in symptoms after just ten weeks of the program. That improvement remained constant throughout the rest of the study.
This could help reduce the number of people who rely on medications to manage their chronic pain.
Before doctors stopped prescribing painkillers, opioids were dispensed to up to 900,000 veterans a yearOverdose deaths among veterans increased by 53 percent between 2010 and 2019, according to 2022 New York University research.
These trends have sparked a broader movement within the veterans administration. Develop programs that treat chronic pain without medications.
Previous studies have shown that mindfulness can help people cope with anxiety and depression. In addition, A 2015 study A study by anesthesiologists at the University of California, San Diego, suggested that mindfulness might reduce the intensity of pain someone feels.
But sometimes, mindfulness meditation practices are expensive and time-consuming.
That’s why this new study looked to see if lower-cost mindfulness methods might still help people cope with pain.
Between 2019 and 2021, the prevalence of chronic pain among American adults ranged from about 20 percent to nearly 22 percent.
There was little or no difference in outcomes between the group that took classes alone and the group that took classes together.
Dr. Burgess wrote that this was “somewhat surprising” because typically, studies of veterans’ psychological well-being suggest that social support is important.
The study authors noted that they could not rule out the effects of other treatments and it is unclear whether people in the mindfulness groups were also using traditional therapies, such as counseling or medications.
But, they wrote, most chronic pain treatments incorporate multiple strategies, so this could be an important way to help people manage their pain, Dr. Burgess said.
She concluded: “Telehealth-based MBIs, which require relatively few resources, could help accelerate and improve the implementation of nonpharmacological pain treatment in health care systems.”

