A major study has found that some new migraine drugs are no more effective than paracetamol in treating attacks.
A comprehensive analysis by researchers at Oxford University concluded that a class of cheaper drugs, known as triptans, were the most effective oral treatment.
They typically cost about a pound a pill and outperform newer drugs, gepants, in suppressing pain during attacks, which affect up to 190,000 people every day.
Experts say triptans are “underused” and should be made more widely available to millions of patients.
But the Migraine Trust said it was often “a painful process of trial and error” to find what works for each individual and urged doctors not to rule out other medications.
One analysis found that all of the drugs were more effective at relieving migraine pain after two hours than placebo, and most relieved pain for up to 24 hours.
The scientists analyzed 137 controlled trials involving nearly 90,000 patients who were given one of 17 drugs or a placebo.
These included triptans: eletriptan, rizatriptan, sumatriptan, and zolmitriptan, which constrict blood vessels in the brain and reduce the release of inflammatory chemicals.
A new range of drugs have also been tested, including ubrogepant, atogepant and rimegepant or “gepants,” which bind to a protein released by nerves at the start of a migraine attack.
These can cost up to 12 times more than triptans, and are estimated to cost around £12 per pill.
All were compared with paracetamol and anti-inflammatory painkillers for pain relief during an attack.
The analysis found that all of the drugs were more effective at relieving migraine pain after two hours than placebo, and most relieved pain for up to 24 hours.

Migraines are estimated to affect almost 10 million adults in the UK, disproportionately affecting women.
Eletriptan is most effective at relieving pain at two hours, followed by rizatriptan, sumatriptan, and zolmitriptan.
The most effective at relieving pain for up to 24 hours were eletriptan and ibuprofen, according to findings published in the BMJ.
Lead author Andrea Cipriani, professor of psychiatry at the University of Oxford, said: ‘We found that all of the licensed drugs are better than placebo, but some are better than other active drugs for the acute treatment of migraine, which is something new.
‘These drugs are four triptans: eletriptan, rizatriptan, sumatriptan and zolmitriptan. They are more effective than the other drugs and are also better than the more recently marketed and more expensive drugs.’
He added: “The efficacy of the new drugs is comparable to that of paracetamol. They are better than sugar pills, but less than the four triptans.”
‘This is important information to keep in mind due to the higher costs of these new treatments.’
Migraines are estimated to affect almost 10 million adults in the UK, disproportionately affecting women, with symptoms including severe headaches, visual disturbances, nausea and vomiting.
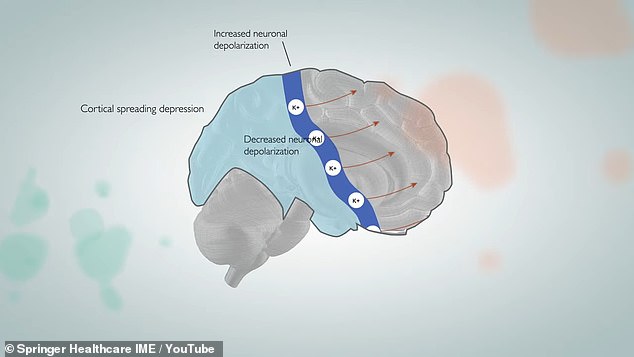
Before some people feel a migraine, their vision is disrupted. This happens when a wave of signals passes through the brain, as in the illustrated diagram. With these signals, a fluid carrying migraine-causing proteins is diverted out of the brain and toward pain receptors.
Medicines regulator Nice recommends eletriptan and rizatriptan for treating migraine, and sumatriptan and zolmitriptan for treating migraine and cluster headaches.
It also gave the green light to rimegepant last year to treat up to 145,000 adults for whom three previous treatments had failed.
Robert Music, chief executive of the Migraine Trust, said triptans “can be very effective for some people” but many do not respond to them or cannot take them because of conditions such as cardiovascular disease.
He said: ‘Finding a migraine treatment that works can be incredibly difficult and can take many years of painful trial and error, the consequences of which can lead to job loss, impact on finances and a significant reduction in mental health.
“Our goal should not be to deprioritize newer treatments, but to make them more available when people need them, so they have greater options and choice.”
Dr Eloisa Rubio-Beltran, a research associate at the Migraine Trust, said more research was needed to test the effectiveness of the drugs against each other in real-world situations.
She said: “The involvement of people with lived experience of migraine in the design of this study should set a precedent in the field and become the norm in future studies.”

