Cervical cancer survival can be increased by 40 percent using a new treatment regimen of existing drugs, according to a large trial.
Giving a chemotherapy booster before standard treatment can also reduce the risk of the disease coming back by more than a third.
Researchers at University College London (UCL) say the “remarkable” findings mean it should become the standard treatment for the disease.
A combination of chemotherapy and radiation therapy, known as chemoradiation, has been the standard treatment for cervical cancer since 1999.
But despite improvements in care, the cancer, which typically affects women in their 30s, returns in up to 30 percent of cases.
Big Brother star Jade Goody died in 2009, a year after her cervical cancer diagnosis; The mother of two children was only 27 years old. After her death, the number of women seeking cervical screening tests, also known as smear tests, increased by about 500,000. This was called “the Jade Goody effect.” The number of attendees at screenings has fallen again

Oscar-winning actress Olivia Colman appeared in a recent film for Jo’s Cervical Cancer Trust, the campaign to raise awareness of the disease which affects more than 3,000 British women a year.

Cervical cancer is one of the most preventable types of cancer, but statistics show that one in three women does not accept the invitation to be screened.
Funded by Cancer Research UK and the UCL Cancer Trials Centre, the trial looked at whether a short course of induction chemotherapy before chemoradiation could reduce relapses and death among patients with cervical cancer that had not spread to other organs.
They recruited 500 patients over 10 years in hospitals in the United Kingdom, Mexico, India, Italy and Brazil.
Patients were randomly assigned to receive the standard treatment or the new treatment combination.
The new treatment program led to a 40 percent reduction in the risk of death and a 35 percent reduction in the risk of the cancer coming back for at least five years.
The results, published in The Lancet, are so clear that experts are calling for the regimen to be used across the UK and internationally.
Dr Mary McCormack, principal investigator of the trial from UCL Cancer Institute and UCLH, said: “This approach is a simple way to make a positive difference, using existing medicines that are cheap and already approved for use in patients.”
“It has already been adopted by some cancer centers and there is no reason why it could not be offered to all patients undergoing chemoradiation for this cancer.”
After five years, 80 percent of those who first received a short course of chemotherapy were alive and 73 percent had not seen their cancer return or spread.

Michelle Keegan, pictured, Louise Rednapp and Nadia Sawalha have also appeared in cervical cancer screening campaigns.
Cervical cancer symptoms to look out for include unusual vaginal bleeding, pain during sex, and lower back or pelvic pain.
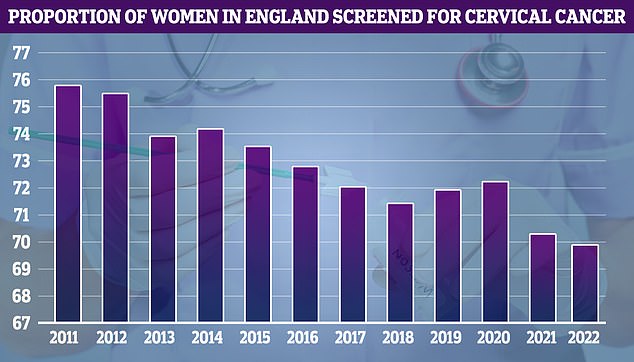
NHS cervical screening data, dating back to 2011, shows that uptake reached its highest level that year (75.7 per cent) and has fallen over time.
In the standard treatment group, 72 percent were alive and 64 percent had not seen the cancer come back or spread.
The researchers said five patients involved in the trial have been disease-free for more than 10 years.
Dr Iain Foulkes, executive director of research and innovation at Cancer Research UK, said: “When treating cancer, timing is everything.
‘Simply adding induction chemotherapy to the start of chemoradiation treatment for cervical cancer has produced remarkable results in the Interlace trial.
‘A growing body of evidence shows that additional chemotherapy before other treatments, such as surgery and radiotherapy, can improve patients’ chances of treatment success.
“Not only can it reduce the chances of cancer coming back, but it can also be administered quickly, using drugs that are already available around the world.”
Around 2,700 women are diagnosed with cervical cancer each year in England and 850 die from it.
The NHS wants to eliminate cervical cancer by 2040 by boosting the uptake of HPV screening and the vaccine, which protects against the virus that causes almost all cases.
The cervical exam, once called a smear test, is a test to check the health of the cervix and help prevent cervical cancer and is offered to women ages 25 to 64.
The most recent figures show only 66 percent of the 11 million eligible women aged 25 to 49 attended their exam, while the proportion was 74 percent among women aged 50 to 64.

