It is the third leading cause of death in the United States, killing more people than dementia and affecting as many as cancer.
Yet millions of Americans have never heard of it.
Sepsis has been called the “silent killer” for this reason. It occurs when the body overreacts to an infection, causing the immune system to go into overdrive and violently attacking healthy tissue.
Another reason for its name is that it often begins with seemingly benign symptoms: fever, fatigue and shortness of breath, to name a few.
But within hours, it can lead to multi-organ failure, heart attacks and amputations.
Now, new data from the CDC has found that the disease is increasing in small but noticeable ways, with the most vulnerable states being the South and Appalachia, as well as wealthy states along areas of the East Coast.
The latest sepsis data from the CDC has shown a slight increase in sepsis deaths over the past three months, which experts warn could be due to the lack of a cohesive sepsis strategy in the US.

Sepsis can affect patients of any age, including three-year-old Beauden Baumkitchner, who had both legs amputated after scraping his knee and contracting staph bacteria.
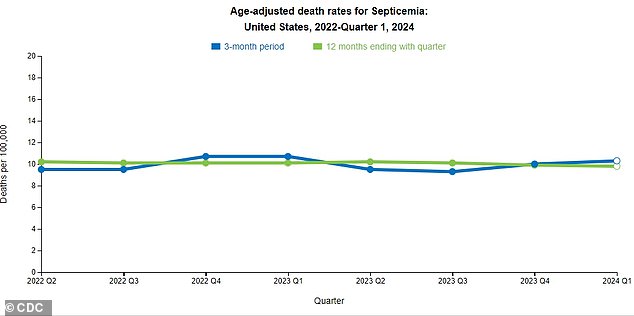
He datafrom the CDC’s National Center for Health Statistics, analyzed sepsis death rates from late 2022 through 2024.
Overall, sepsis deaths have shown a slight uptick, from 9.3 cases per 100,000 to 10.3 cases per 100,000, an increase of just under one percent.
Between 2022 and 2024, men were consistently more likely to die from sepsis, with a mortality rate of 11.5 per 100,000 in the first quarter of 2024, compared with 9.4 per 100,000 in women.
Most age groups have remained stable over the past two years, but those aged 85 and older have seen an increase from 141 per 100,000 in the third quarter of 2023 to 166 per 100,000 so far in 2024.
In the first quarter of 2024, Southern and Appalachian states recorded the highest number of sepsis deaths. Louisiana had the most, at 18 per 100,000, followed closely by Kentucky and Arkansas, at 17 per 100,000.
While these states are historically prone to chronic diseases like obesity, diabetes and cancer — all risk factors for sepsis — wealthier states along the East Coast also saw higher numbers of sepsis cases.
New Jersey, for example, has a sepsis mortality rate of 16 per 100,000, followed closely by Maryland and Pennsylvania, at 14 and 13 per 100,000, respectively.
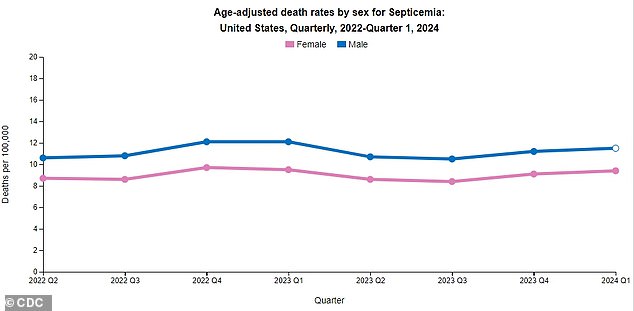
According to the CDC, men have been consistently more likely to die from sepsis compared to women.
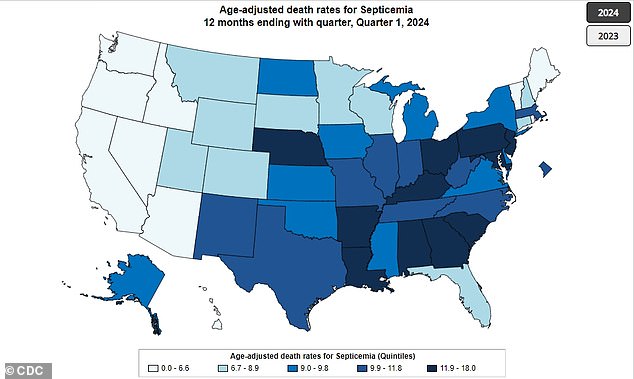
The map above shows the average sepsis death rates in each US state per 100,000 people.
Experts have suggested that the steady rise of the disease, which causes the immune system to overreact to an infection and attack healthy organs, could be due to a lack of cohesive medical care in the US.
Unlike the United Kingdom, Australia, and several other countries, the United States does not have a national sepsis protocol. In fact, CDC data from 2023 found that more than 1,400 hospitals (about a quarter) in the US have no sepsis program at all.
And of those, just over half dedicate staff time to focus on developing the sepsis protocol.
However, new CDC data shows the number of hospitals with a sepsis program rose from 73 percent to 78 percent between 2022 and 2023.
“Doctors are not given enough information to help them diagnose sepsis,” Dr Steven Simpson, a professor of medicine at the University of Kansas and president of the nonprofit Sepsis Alliance, previously told DailyMail.com.
‘There is no catchy phrase that helps doctors and hospitals detect it, as there is in other countries.
“Every hospital in the country should have a sepsis committee, a quality improvement program, and organize their facilities to be prepared to detect and treat sepsis. At present, this is not the case at all.”
Sepsis affects more than 1.7 million Americans each year. This number is comparable to that of cancer, which is diagnosed in 1.9 million people and is also increasing across the United States.
Sepsis kills more than 350,000 people each year, or one person every 90 seconds. Only cancer and heart disease kill more people in the United States, with 600,000 and 700,000 deaths, respectively.
While these diseases primarily affect older people, what makes sepsis so scary is that it can affect anyone.
People aged 65 and older tend to be the most vulnerable, although around 75,000 patients each year are under 18.
It is also the leading cause of death in hospital, accounting for one in three.
According to the Sepsis Alliance, sepsis claims more lives “than those killed by stroke, prostate cancer, breast cancer and opioid overdose combined.”
Worldwide, this disease is responsible for one in five deaths (20 every minute) and outnumbers cancer.
But despite how terrifyingly common the disease has become, one in three Americans has never heard of it, the Sepsis Alliance found.
And sepsis isn’t even included on the CDC’s list of “Leading Causes of Death,” though it’s not clear why.
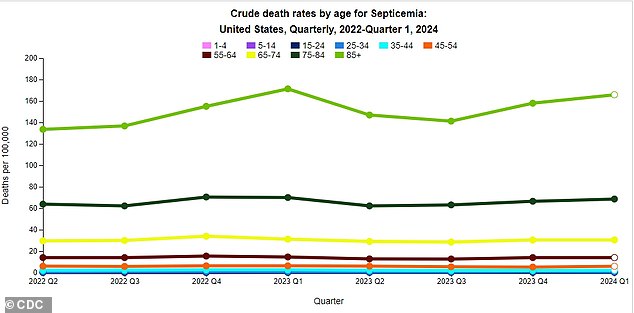
The graph below shows that people aged 85 years and older have shown the largest increase in sepsis deaths over the past two years.
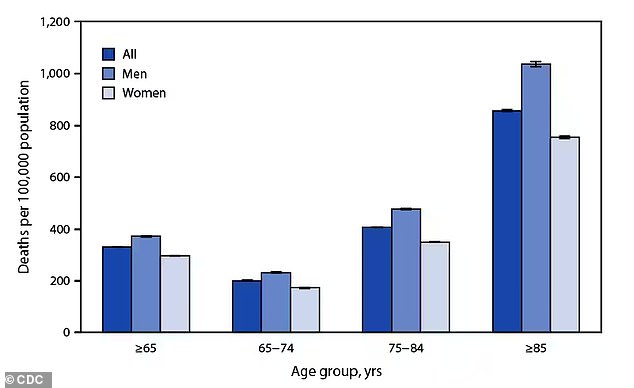
Most patients with sepsis are over 85 years old, although it is known to affect patients as young as infants.
Lack of awareness can make it difficult for patients to identify the condition and seek help immediately, sepsis survivor Don Smith previously told DailyMail.com.
Mr Smith, now 67, suffered sepsis in 2017 after becoming infected with strep throat, unaware of the extreme reaction taking place in his body.
But within a few days, her foot became so swollen that she couldn’t get out of bed. Several of her toes had to be amputated, as they had turned black due to lack of circulation.
Until then, she had only a vague idea of what sepsis was. And several other patients she met told her that their doctors just told them “you were very sick” instead of telling them they had sepsis.
“Use the word sepsis. Tell people what it is and what it means, because I’d heard the word sepsis before, but I had no idea what it was,” Smith said.
“And I almost died from it. We need to spread the word so that fewer people die.”

“Use the word sepsis. Tell people what it is and what it means, because I’d heard the word sepsis before, but I had no idea what it was,” Smith said. “And I almost died from it. We need to get the word out there so that fewer people die.”

Sepsis also carries the risk of repeated hospitalisation, as it can cause permanent organ damage and other long-term effects. Chloe Cummings (left) and her mother Kimberly have contracted sepsis about 18 times in total and are at constant risk of being hospitalised.
Another danger is that sepsis can leave the body more vulnerable to repeated episodes: Sepsis Alliance, for example, estimates that one-third of sepsis survivors end up back in the hospital within three months, usually due to repeated episodes.
In many patients, sepsis causes permanent damage to organs such as the lungs, brain and heart, which requires long-term maintenance and can result in repeated hospitalizations.
A new study published this week in the journal American Journal of Critical Care MedicineFor example, of 7,100 patients with sepsis, nearly one in four was readmitted to the hospital within 30 days.
Of these, two-thirds were due to repeated episodes of sepsis and almost half to infections.
Priscilla Hartley, a co-author of the study and an assistant professor of nursing at Augusta University in Georgia, said that in nine out of 10 cases, readmission occurred in patients “deemed well enough to be discharged home or to receive home health care.”
Chloe Cummings, 30, has suffered from sepsis more than a dozen times since she was a baby. Her mother previously told DailyMail.com that sepsis attacked her daughter’s bones, landing her in the hospital frequently because something as innocent as falling off a swing could result in a fracture or dislocation.
“It’s just a reminder that you don’t come out of this unscathed,” Cummings said.