A 60-year-old German man has likely been “cured” of HIV, a medical milestone achieved by only six other people, doctors have announced.
The man was treated for acute myeloid leukemia, a type of blood cancer that begins in young white blood cells in the bone marrow, with a stem cell transplant.
The painful and risky procedure is intended for people with HIV and aggressive leukemia, so it is not an option for nearly all of the nearly 40 million people living with the deadly virus worldwide.
According to doctors, he now appears to be free of both cancer and HIV.
The German, who remains anonymous, was dubbed “Berlin’s next patient.”
Timothy Ray Brown with his dog, Jack, at Treasure Island in San Francisco in 2011. Brown, known for years as the Berlin patient, received a transplant in Germany from a donor with a natural resistance to the AIDS virus. It was believed to have cured Brown’s leukemia and HIV.
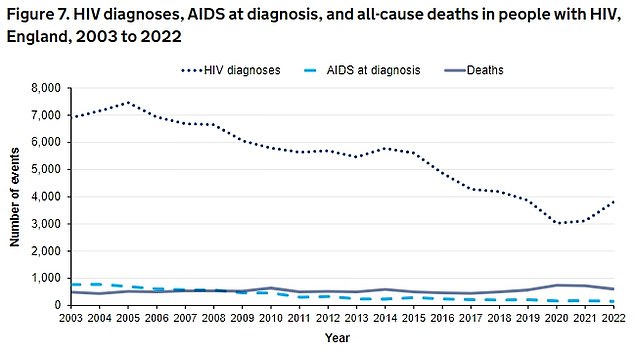
Latest UKHSA data shows HIV diagnoses rose by 22 per cent – from 3,118 in 2021 to 3,805 in 2022
The original Berlin patient, Timothy Ray Brown, was the first person declared cured of HIV in 2008. Brown died of cancer in 2020.
The second man from Berlin to achieve lasting remission from HIV has been announced ahead of the 25th International AIDS Conference in Munich next week.
He was first diagnosed with HIV in 2009, according to the research summary presented at the conference.
The man received a bone marrow transplant for his leukemia in 2015. The procedure, which has a 10 percent risk of death, essentially replaces a person’s immune system.
He then stopped taking antiretroviral drugs, which reduce the amount of HIV in the blood, in late 2018.
Nearly six years later, he appears to be free of both HIV and cancer, medical researchers said.
Christian Gaebler, a research physician at Berlin’s Charité university hospital who is treating the patient, said the team could not be “absolutely certain” that every last trace of HIV had been eradicated.
But “the patient’s case is highly indicative of an HIV cure,” Gaebler added.
“He feels good and is excited to contribute to our research efforts.”
There are an estimated 105,200 people living with HIV in the UK, according to the National AIDS Trust.
But only 94 percent of these people are diagnosed.
This means that around 1 in 16 people living with HIV in the UK do not know they have the virus.
International AIDS Society President Sharon Lewin said researchers are hesitant to use the word “cure” because it’s not clear how long they need to follow up on such cases.
But more than five years in remission means the man “would be close” to being considered cured, he told a news conference.
There is an important difference between the man’s case and that of other HIV patients who have achieved long-term remission, he said.
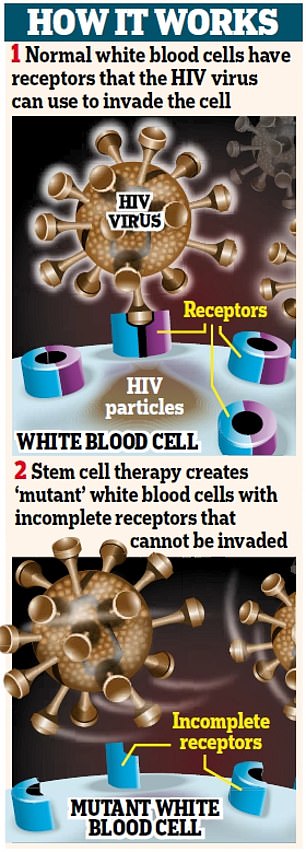
All but one of the patients received stem cells from donors with a rare mutation in which part of their CCR5 gene was missing, preventing HIV from entering their body’s cells.
Those donors had inherited two copies of the mutated CCR5 gene (one from each parent), making them “essentially immune” to HIV, Lewin said.
But the new patient in Berlin is the first to receive stem cells from a donor who had inherited only one copy of the mutated gene.
About 15 percent of people of European descent have one mutated copy, compared with one percent who have both.

There are an estimated 105,200 people living with HIV in the UK, according to the National AIDS Trust (stock)

Timothy Ray Brown poses for a photograph on Monday, March 4, 2019, in Seattle. Brown, also known as the “Berlin patient,” was the first person to be cured of HIV infection.
Researchers hope the latest success will mean there will be a much larger pool of potential donors in the future.
The new case is also “promising” for the broader search for an HIV cure that works for all patients, Lewin said.
“This is because it suggests that you don’t actually need to remove every piece of CCR5 for gene therapy to work,” he added.
The Geneva patient, whose case was announced at last year’s AIDS conference, is the other exception among the seven. He received a transplant from a donor without any CCR5 mutations, but still achieved long-term remission.
This showed that the effectiveness of the procedure was not due to the CCR5 gene alone, Lewin said.
Mr Brown, the first “cured” patient, was diagnosed with HIV while studying in Berlin in 1995.
A decade later, he was diagnosed with leukemia, a cancer that affects the blood and bone marrow.
Acute myeloid leukaemia is the most common type among adults: around 3,000 Britons and 20,000 Americans are diagnosed each year.
It is also the deadliest, claiming 2,700 lives each year in the UK and 11,000 in the US.
To treat his leukemia, his doctor at the Free University of Berlin used a stem cell transplant from a donor who had a rare genetic mutation that gave him natural resistance to HIV, hoping to eliminate both diseases.
It took two painful and dangerous procedures, but it was a success: in 2008, Brown was declared free of both ailments and was initially dubbed “the Berlin Patient” at a medical conference to preserve his anonymity.
Two years later, she decided to break her silence and became a public figure, giving speeches and interviews and starting her own foundation.
“I am living proof that there could be a cure for AIDS,” he told AFP in 2012. “It’s wonderful to be cured of HIV.”
Although he remained cured of HIV, the cancer returned.
Ten years after Brown was cured, a second HIV patient, nicknamed “the London Patient,” found himself in remission 19 months after undergoing a similar procedure.
The patient, Adam Castillejo, is currently HIV-free.
Other patients include a Dusseldorf patient in 2023, a New York patient in 2022, the Esperanza patient in 2021, and Loreen Willenberg in 2020.
Unlike the other patients, in the cases of Patient Esperanza and Mrs. Willenberg, their immune systems naturally eliminate the virus from their bodies.

