<!–
<!–
<!– <!–
<!–
<!–
<!–
Scientists have successfully eliminated HIV from infected cells, which has been hailed as a major breakthrough in the race for a cure.
Using “genetic scissors,” experts were able to extract the virus from infected T cells in the laboratory, removing all traces.
Experts said the hope is the technique could one day be developed into a treatment, ending the need for lifelong antiviral drugs.
HIV integrates into the infected person’s DNA, taking control of the host’s cellular machinery to replicate.

Using “genetic scissors,” they were able to extract the virus from infected T cells in the laboratory, removing all traces (stock)
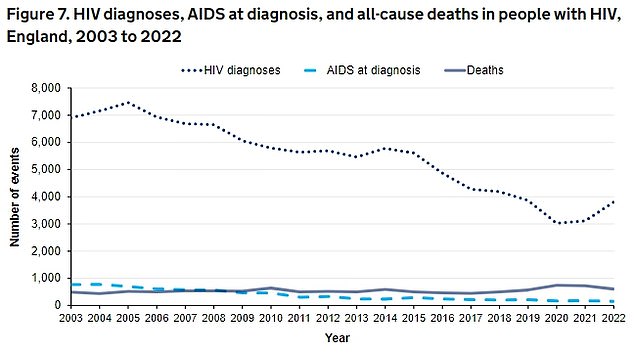
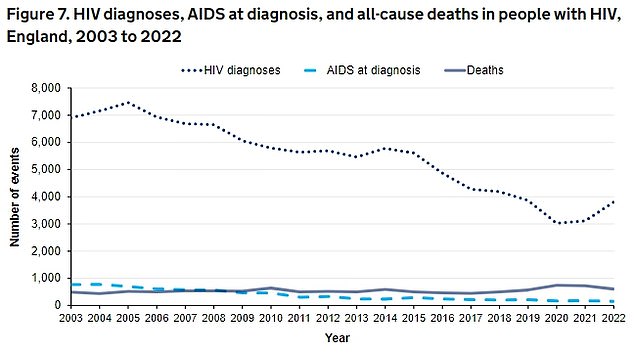
The latest UKHSA data shows that HIV diagnoses increased by 22%, from 3,118 in 2021 to 3,805 in 2022.
Although it can be effectively controlled with antiviral therapies, “reservoirs” of reinfection remain, allowing it to take over if treatment stops.
Scientists want to develop a treatment that could prevent it from escaping the body’s immune system.
Using the Crispr genome editing technique, researchers at UMC in Amsterdam, the Netherlands, identified the part of the virus that is the same in all known strains of HIV.
They were also able to target these “hidden” HIV reservoir cells by focusing on specific proteins found on the surface of these cells.
Writing on the eve of the European Congress of Clinical Microbiology and Infectious Diseases, the authors said “these results represent a crucial step forward towards the design of a cure strategy.”
“While these preliminary results are very encouraging, it is premature to declare that there is a working treatment for HIV on the horizon,” they added.
Lead researcher Dr. Elena Herrera-Carrillo said the hope is to provide a therapy that can effectively combat multiple variants of HIV.
But she added that significant work will be needed to turn the “proof of concept” into a treatment targeting the majority of HIV reservoir cells, which will likely still take years.
It is one of several advances in the field, with the successful use of the technique in monkeys last year leading to recruitment for the first human trials.
Elsewhere, researchers at the University of Pittsburgh School of Medicine say they have identified promising drugs for reversing HIV’s ability to evade detection by the immune system.
Drugs traditionally used on cancer patients, called proteolysis-targeting chimeras, or PROTACs, were able to target a key protein and suppress HIV replication, while showing signs that the immune response could be restored.
Commenting on the research, Dr James Dixon, associate professor of stem cell technologies and gene therapy at the University of Nottingham, said talk of a cure was still some way off.
He said: “Using CRISPR technology to extract or disable the HIV genome is a well-discussed but promising strategy.
“However, the delivery of these systems remains a significant issue and much more work will be needed to demonstrate that the results of these cellular assays can be obtained in a whole body for future therapy.”
