Viewing all obese people as sick is outdated and causes “rampant discrimination,” according to a new book.
Rekha Nath, an associate professor of philosophy at the University of Alabama, says there is enough evidence to show that being fat is not always bad for your health and that the problem is not black or white.
It builds on a wave of new research over the past decade suggesting that our current methods for tackling obesity aren’t working and that a more nuanced approach is needed if we are to create a healthier public.
Professor Nath also argues that these standards contribute to a “collective aversion” towards overweight people that actually makes them more likely to gain weight and become depressed.
A 2023 study found that a person’s fat distribution was more important to their overall fat than just their body weight. Fat around the midsection, which puts strain on crucial organs, led to a higher risk of diseases that could lead to early death.
He argued that changing the way society thinks about obese people will help create better health care practices for them that will make them more likely to lead healthy lives.
“It’s okay to be fat because there’s nothing wrong with being fat. There’s nothing wrong with being fat, of course, except for all the things our society does to make being fat bad,” she said.
In her new book, titled ‘Why It’s Okay to Be Fat’, Professor Nath pointed to a 2010 review of 36 older studies that found overweight people who exercise were less are more likely to die prematurely than unfit people with a “healthy” body weight.
She argues that lifestyle factors, in this case exercise, may be a better predictor of health than waistline alone.

Professor Nath has published several articles on obesity and global social political philosophy and obtained a PhD from the University of Melbourne.
That study and the U.S. health care system use the body mass index (BMI), which classifies people into one of three categories (healthy weight, overweight and obese) based on their height and weight.
For example, someone who is 5 feet 2 inches tall and weighs 153 pounds would be considered overweight, and someone who is 5 feet 2 inches tall and weighs 175 pounds would be considered obese.
But doctors have been increasingly critical of the measure. Fatima Cody Stanford, an obesity specialist at Massachusetts General Hospital and Harvard Medical School in Boston, said BMI does not fully reflect a person’s health.
Not everyone with a high BMI is in poor health: Factors such as fat distribution and activity level may be more important than weight alone, she said.
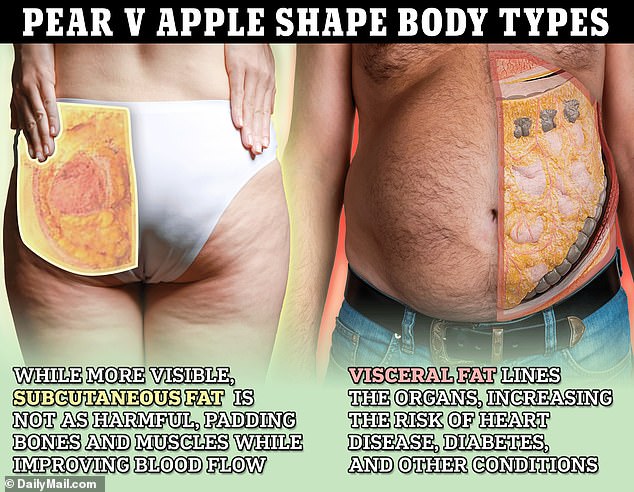
For example, more and more studies are showing that where your fat is located is more important than how much fat you have overall.
Studies have shown that fat located deep in the midsection (overlying the stomach, liver, and kidneys) contributes more to some of the factors associated with obesity than fat located just under the skin in the legs and buttocks.
This is because deep abdominal fat, called visceral fat, releases more molecules that inflame the body, contributing to a host of health problems, than superficial subcutaneous fat, according to Dr. Howard E. LeWineinternist at Brigham and Women’s Hospital.
This association is so clear that a 2023 study found that people who stored most of their fat outside their belly were healthy, making 15 percent of obese people included in the study healthy overall.
“When we only look at height and weight, we know nothing about the individual’s health status,” Dr. Stanford told Nature.
Some doctors will scoff at the idea that being fat is healthy, especially given the current situation.
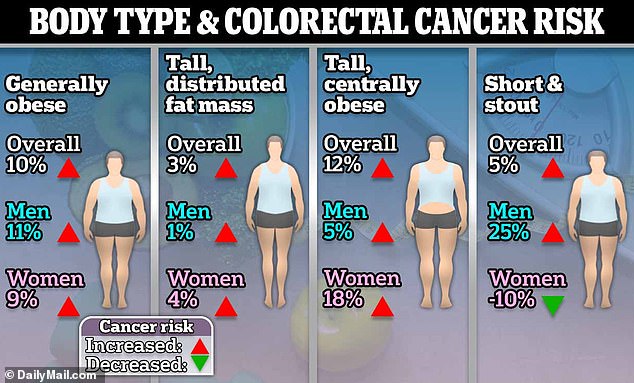
Researchers from six countries, including the United States and the United Kingdom, found that people who were “generally obese,” as well as those who were taller and had more abdominal fat, had the highest risk of colorectal cancer.
According to the NIH, about seven in ten Americans are overweight or obese, a number that has been steadily increasing since the 1970s.
The annual cost of treating obesity and obesity-related conditions in the U.S. likely exceeds $1.4 trillion. a 2020 report from the Milken Institute, a nonprofit think tank.
This includes spending by private insurers, public insurers, and individual costs for bariatric surgeries, medications, diagnostic tests, preventive services, and medical treatment.
Although no one dies directly from obesity, Harvard researchers Obesity-related conditions are estimated to cause nearly 500,000 deaths per year in the United States.
Obesity causes type 2 diabetes, high blood pressure, stroke, heart disease, liver disease, and many types of cancer.
Professor Nath’s book was published by the Taylor & Francis Group, a major academic publisher.
It also causes people to lose, on average, between two and four years of life, making it more closely linked to premature death than smoking, the Harvard researchers said.
Dr Nath acknowledged this, but said that methods to treat obesity do not always work well and instead make obese people feel worse.
Until Ozempic came along, the standard advice for overweight people was to eat less and move more. Sometimes, this works.
But Professor Nath cited a study showing that 41 per cent of people who try to lose weight by dieting end up heavier than their original weight four or five years later.
While diets are not always effective, when people don’t see results they are considered a failure, Professor Nath said.
“Being fat is seen as unattractive, even disgusting. We see fatness as a sign of weakness, of greed, of laziness,” said Professor Nath.
This creates a system where being thin makes people good and being fat makes them bad, she said, adding: “Many, if not most, of us are not quite sure whether it’s actually okay to be fat.”
The amount of fat a person has depends on how many calories they consume, regardless of who they are.
If you consistently consume more calories than your body uses for fuel, your body will begin to store them. excess calories in the form of fat.
However, genetics, stress, medication, and health issues can make fat loss difficult by causing inflammation, creating a slower metabolism, and affecting body fat distribution.
Whatever the cause, it is clear across society that people fear getting fat and associate it with failure, Professor Nath said.
One in three college students said becoming obese would be “one of the worst things that could happen to a person.” A 2014 study It was found at Dickinson College and the Yale University School of Medicine.
Nearly half of 4,000 respondents in a global online survey said they would rather lose a year of their life than become obese, Professor Nath said.
This creates a bias that means fat people receive worse medical care, fewer job opportunities, and are more likely to be shamed in public.
This makes them less likely to lose weight and more likely to develop conditions such as depression and anxiety that harm them.
“Not only does subjecting obese people to weight stigma appear to make them less likely to lose weight, but weight stigma appears to seriously harm their physical and mental health in a number of ways,” Professor Nath said.
This is more common in Western cultures such as the United States, the United Kingdom and Australia, Professor Nath said. But other cultures actually prefer fatness to thinness.
For example, fatness is considered a sign of beauty in communities in Cross River State in southeastern Nigeria.
The solution to the problem is not to ignore a person’s weight when they go to the doctor’s office, Stanford said. BMI still gives doctors “an idea of how much weight a person is carrying,” Stanford said.
The key is that after taking into account a person’s weight, you still have to look at all the other factors in their life to determine their health, he said.