Dear Wes Streeting:
Last week, in the pages of this newspaper, you wrote about the crisis affecting the National Health System. You repeated what you said on the day you were appointed Health Secretary: that the National Health System was “broken”. “Sunlight is the best disinfectant,” you wrote, calling on frontline staff and patients to diagnose the problems so that you could “write the right prescription”.
Well, I’ve worked full-time in the NHS for over 20 years and I can certainly tell you something. I’m genuinely shocked by the state of the health service.
The most important thing is that people are afraid of getting sick, of going to the emergency room, of having to see a GP or having an operation. They are afraid because they fear not getting the treatment they need, when they need it.
There is a huge will among staff to change this situation, but some very bold decisions will need to be made. In the long term, we may need to fundamentally change the NHS – how it works and how it is funded. In the meantime, here is what needs attention now!
Health Secretary Wes Streeting wrote about the crisis consuming the NHS in the Daily Mail last week.
More beds to solve crisis in corridors
In recent years we have tried to save money by reducing the number of hospital beds and moving services out into the community. It doesn’t work. The UK now has a shockingly low number of beds: 2.43 per 1,000 people compared with 5.73 in France and 7.82 in Germany.
Don’t listen to management consultants who tell you that’s the answer. You said you wanted to know if patients “are being left unattended, on stretchers in hallways for hours.” Go to any emergency department and see for yourself. It’s happening now.
Eliminate university fees
There simply aren’t enough frontline staff. We need to encourage the best to train and retain them when they graduate. Tuition fees for nursing and medical students should be scrapped and a full bursary reinstated. In return, they have to commit to working in the NHS for a minimum of, say, seven years.
This will help restore the sense of loyalty and duty that existed in my generation of doctors (who paid no fees and received grants) but is often lacking in the younger generation (who did pay). Resist the temptation to fill the gaps with junior doctors – it takes years to train a doctor for some reason and I am concerned about patient safety as PAs bear the brunt of it.
Give management a blow
There are many layers of management doing very little for patient care, and we, as physicians, spend too much time filling out forms that are useless to them.
A consultant friend says that the hour and a half it takes to complete NHS paperwork after a patient’s assessment takes just 20 minutes in the private sector. When working in the private sector, all you have to do is write a letter to the patient’s GP.
It’s interesting that when time is money, all these forms become obsolete and unnecessary.
Whole layers need to be removed. There is no excuse for having managers who only manage managers. Those who survive should spend the equivalent of one day a week on the front line. This already happens in some trusts – where I work, for example, the medical director spends one day a week in the dementia service assessing patients. It should be mandatory across the NHS.
Make waiting lists your top priority
These problems are out of control. There is no magic solution, but increasing beds, staff numbers and efficiency will help. Use the private sector in the short term, but be careful not to rely on it for too long because it will increase costs.
Eradicate the slackers
Midwives have been reintroduced, but we need them on the wards, driving care, not in the back offices where they spend much of their time.
It should be much easier to fire employees who don’t do their part or don’t care about their jobs. And we need strong protections for whistleblowers.
In some areas, there has been a real deterioration in attitude and productivity since the pandemic, with some employees becoming accustomed to doing less. It’s a painful truth to acknowledge, especially when so many are working themselves to exhaustion, but the slackers need to be rooted out.
Stricter targets for A&E
Emergency departments are often chaotic. Various policies have attempted to improve this and the “four-hour rule”, which states that 95 per cent of patients must be seen and treated within four hours, certainly helps to focus attention.
I think it is more than reasonable to ensure that, from the moment someone checks in at reception, they do not wait more than an hour before being seen and, if they require more complex care, they are admitted or referred elsewhere within those four hours.
Placing other specialists in primary care physicians’ offices
GPs are the scapegoats: everyone blames them for the problems of the National Health System, but most of them work very hard. Is it any wonder that so many stop working?
Yes, it is sometimes almost impossible to get an appointment. We need to encourage more young doctors to go into primary care and we need to think creatively about how to retain them.
In my opinion, psychiatrists have been incorporated into GP surgeries to see patients with mental health problems and offer support for less acute psychological diagnoses. This is a brilliant idea and means fewer referrals to secondary mental health services. Surely something like this can be implemented across the country, and with other disciplines?
Those suggestions are just the beginning, Wes. I’m sure there will be readers who can tell you their own stories, and plenty who will have clever and clever solutions.
I trained as a doctor because I wanted to work in the National Health Service. I hate to see it on its knees. Please do the best you can. We may not agree on everything politically, but from the bottom of my heart I wish you success.
Maximum
Strictly pits celebrities against professionals
The Strictly saga reaches its climax today with the publication of the BBC’s verdict on the dispute between professional dancer Giovanni Pernice and actress Amanda Abbington. Whatever the verdict, the mental health of both has been affected and the Corporation urgently needs to protect future contestants.
Perhaps the problem lies in the culture shock behind the show. Professional dancers need very different personality traits than celebrities. Discipline is paramount. Dedication to their skill consumes their lives. The professional dancers I know tolerate training and a lifestyle that few would be able to endure. To some, it may even seem sadistic, but to the dancers, it is a means to an end, a necessary sacrifice for their art.
Celebrities are motivated by different things: adulation, adoration, the spotlight.
I wonder how many understand the difference before signing up for the programme and whether the BBC prepares them for it.
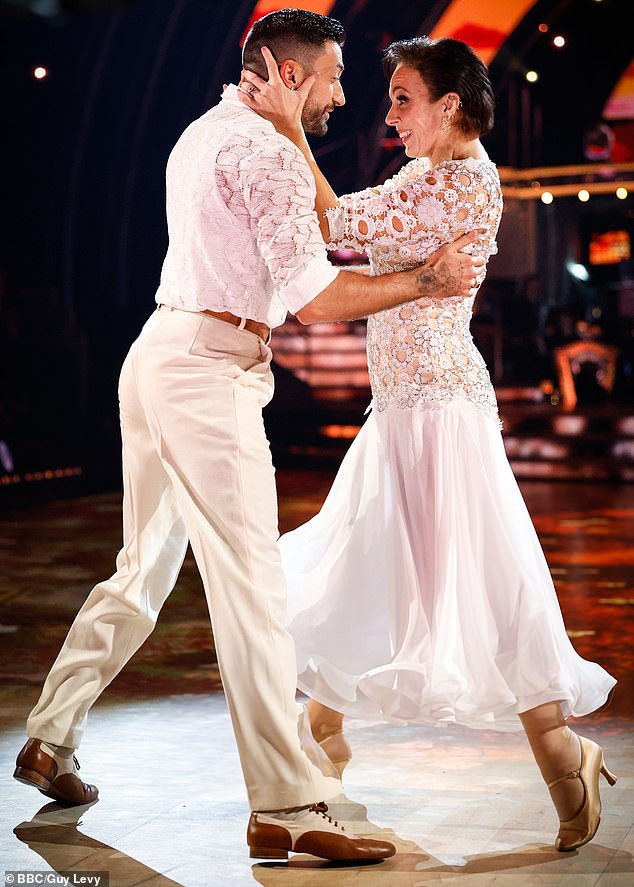
The BBC’s verdict on the dispute between professional dancer Giovanni Pernice and actress Amanda Abbington will be announced today
One in ten people have continence problems. But how often do you hear someone talk about it?
Now the estimated eight million Britons living with overactive bladder (a cause of incontinence) could have a new lease on life after authorities approved the drug vibegron.
We need to lose the shame around this problem and offer ourselves the appropriate treatment.
Dr. Max prescribes… Blood donation
The National Health Service has issued an alert saying it is running low on blood following the recent cyber attack which led to the postponement of thousands of operations. The stock of O negative blood stands at 1.6 days, compared to 4.3 days for all blood types.
People with O negative and O positive blood (the most common types) have been urged to donate.
Sign up and book an appointment on the GiveBloodNHS app or at www.blood.co.uk.

