A new form of mpox is spreading in the Democratic Republic of the Congo (DRC), raising fears it could spread to Europe.
The clade 1b mutation, which experts call “the most dangerous yet,” is believed to be behind a wave of miscarriages and kills one in ten infected people.
Scientists tracking the spread of the new strain have already warned that it appears to be the most transmissible yet and could even end up in Europe.
So how concerned should we be, who is most at risk, and what (if anything) should we do to protect ourselves?
Here MailOnline explains everything you need to know.
Mpox, formerly known as monkeypox, is a rare viral infection that people commonly contract in tropical areas of west and central Africa. Pictured, a colored transmission electron micrograph of monkeypox particles (green) found inside an infected cell (pink and purple).
What is mpox?
Mpox, formerly known as monkeypox, is a viral infection that was once confined primarily to western and central Africa.
It was transmitted to humans through direct contact with animals such as squirrels, which are known to harbor the virus.
However, it can also be transmitted through very close contact with an infected person.
The virus was first discovered when an outbreak of a smallpox-like disease occurred in monkeys kept for research in 1958, hence the earlier name.
The first human case was recorded in 1970 in the Democratic Republic of the Congo and since then the infection has been reported mainly in countries in central and western Africa.
In 2022, an outbreak in Europe and the United States primarily affecting gay and bisexual men led the World Health Organization (WHO) to declare a public health emergency.
It was the first time it was reported that mpox was spread primarily through sexual contact.
What is the new strain?
Clade 1b is a descendant of the deadly clade 1 mpox strain and is different from the milder version (clade 2) that spread to more than 20 countries, including the United Kingdom, in 2022.
Once again, sexual transmission appears to be the main way clade 1b spreads, and researchers believe the current outbreak began in a bar used by sex workers.
The disease first appeared in the rainy season, when roads were in poor condition and the movement of people between cities and villages was limited.
Scientists have warned that the current dry season could lead to increased transmission, particularly during the school holidays as people move around more.
In a briefing for journalists yesterday, Trudie Lang, a professor of global health research at the University of Oxford, said that when the outbreak was detected in the Democratic Republic of the Congo last September, scientists had assumed it would be clade 2, due to sexual transmission.
However, genetic testing revealed that it belonged to the most virulent strain.
Historically, clade 1 has only been found in people who eat infected bushmeat, and transmission is largely limited to the affected household.
How is it different from other strains?
Scientists have warned the strain was “without a doubt” the “most dangerous” yet.
It is also unclear how quickly the new strain spreads.
Like Clade 2, Clade 1b causes a severe blister-like rash at the site of infection.
But the symptoms are more severe and the rash usually spreads to the entire body.
So far, around 600 patients with the mutant form of the virus have been identified in Kamituga, the city where it was first detected.
Leandre Murhula Masirika, research coordinator for the health department of South Kivu province in the east of the country, said 24 of the country’s 26 provinces were affected by the outbreak.
However, experts warn that the real figure could be much higher, as hospitals are only recording severe cases requiring advanced care.
The number of asymptomatic cases or people with minimal symptoms, who could still spread the infection, is also still unknown.
Where has the mutant form of the virus been found?
So far, all cases have been reported in cities in the Democratic Republic of the Congo that border the nations of Rwanda, Burundi and Uganda.

After clade 2 sparked alarm among global health officials in 2022, new infections gradually declined amid heightened awareness of the disease and a rushed vaccination program. At the time, the United Kingdom reported nearly 4,000 cases, and England’s National Health Service inoculated more than 68,000 people against the disease with the smallpox vaccine. In the photo, long lines to receive the vaccine.

The smallpox vaccine works because the two viruses are closely related. But experts said there was not yet enough evidence to suggest a vaccine would be effective against this new strain.
However, scientists said it was highly likely that the virus had already reached these neighboring countries, although no cases have been confirmed outside the Democratic Republic of the Congo.
John Claude Udahemuka, a professor at the University of Rwanda who is monitoring the outbreak in the Democratic Republic of the Congo, said they believe the first person with the new strain was a man who had sex with a woman in the town of Kamituga.
She then met with other women in several different locations.
Scientists warned that sex workers regularly travel between the Democratic Republic of the Congo and its neighbors, meaning this could be a potential route of transmission.
How deadly is it?
Mpox is usually not serious and most patients recover within a few weeks without treatment. However, the disease can be fatal.
Early estimates indicate that the new mutant strain has a mortality rate of five percent for adults and ten percent for children.
But another worrying aspect is that the infection in pregnant women was causing an “alarming” number of spontaneous abortions.
Experts also said that some cases had even led to irreversible vision loss, as well as recurring skin rashes all over the body.
Earlier this month, the WHO said the mpox outbreak in the Democratic Republic of the Congo was “concerning.”
He pointed to limited public awareness about mox, a lack of treatment kits and vaccines and many other health priorities of the country as factors in the emergence of a new strain.
The risk associated with MPOX in the Democratic Republic of the Congo “remains high,” he added.
How is it spread?
Mpox is not classified as a sexually transmitted infection, although it can be transmitted through direct contact during sexual intercourse.
Contagious lesions, through which infections are most likely to be transmitted, can appear anywhere on the body.
The infection can also be transmitted through contact with clothing or bedding used by an infected person.
What are the symptoms people should watch out for?
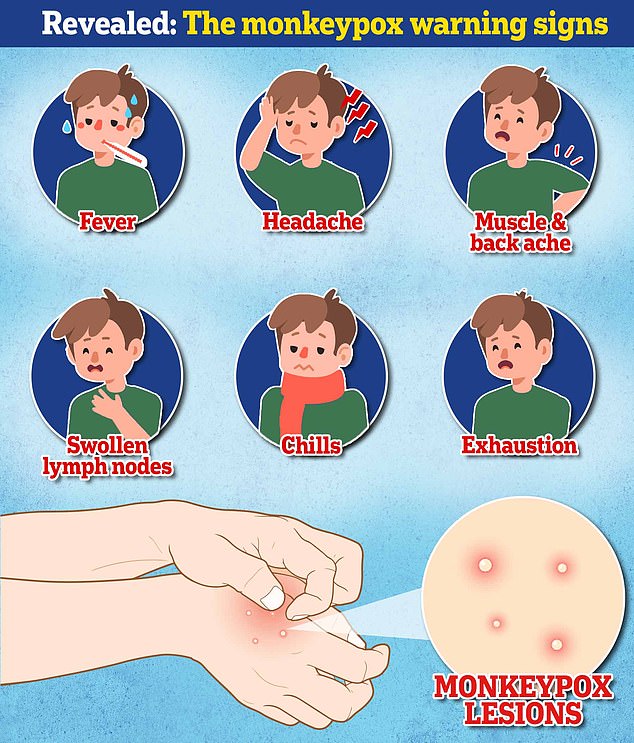
Initially, mpox causes a flu-like illness: fever, headache, muscle pain, back pain, swollen lymph nodes (glands found in the neck, groin, or under the arms), and fatigue.
Within one to five days, a rash appears, usually first on the face and then spreading to other parts of the body, including the genitals.
The rash is similar to chickenpox. It starts as raised spots that later turn into small fluid-filled blisters. These blisters turn into scabs that eventually fall off.
The illness can last up to four weeks, but most cases go away on their own without treatment.
During the latest outbreak, the UK Health Security Agency warned anyone with unusual rashes or lesions on any part of the body, in particular gay or bisexual men, those who have been in contact with someone who has or might have mpox , and anyone who traveled to West Africa in the last three weeks to contact NHS 111 or call their local sexual health service.
What happens if someone tests positive in the UK?
If a person is suspected of having monkeypox in the UK, they will normally be given a PCR test, similar to those used to detect Covid.
These use swabs taken from the skin and throat.
There are no specific treatments and the NHS currently says that if symptoms are mild, patients may simply be advised to stay at home until they recover.
If the disease is more severe, patients may be offered treatment that includes antiviral drugs: Tecovirimat, designed for smallpox, and Cidofovir.
Will the current vaccine work against this?
After clade 2 sparked alarm among global health officials in 2022, new infections gradually declined amid heightened awareness of the disease and a rushed vaccination program.
At the time, the United Kingdom reported nearly 4,000 cases, and England’s National Health Service inoculated more than 68,000 people against the disease with the smallpox vaccine.
This works because the two viruses are closely related.
But experts said there was not yet enough evidence to suggest a vaccine would be effective against this new strain.
Trials will be needed to resolve this, which will take time, they added.

