Infant deaths are at a record high in the U.S. for the second year in a row and are much higher than in peer countries.
A new CDC report showed there were 5.61 per 1,000 deaths among babies under one year old in 2023, about the same level in 2022, which officials expected to be a blip.
The rate in the United States is up to 75 percent higher than in countries like the United Kingdom and Australia, and experts blame the growing maternal health crisis in the United States.
The leading causes of infant death were birth defects, disorders related to premature birth, sudden infant death syndrome, accidental injuries and maternal illnesses.
But there were huge disparities between the states. Mississippi, Arkansas, Louisiana, Ohio and Oklahoma had rates between seven and nine deaths per 1,000 births.
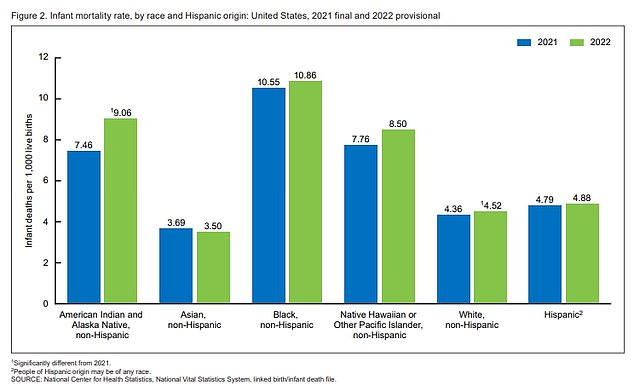
Black babies were found to have twice the risk of dying during their first year of life, which experts attribute to poorer maternal health care for Black women and a lack of access to doctors in many predominantly Black areas.
Other experts attribute poor outcomes for all babies to a lack of national insurance, causing poorer mothers to miss doctor’s appointments before and after birth.
This can cause deadly diseases to go undetected. For example, in 2023, the CDC reported that cases of babies born with syphilis had increased tenfold in a decade.
If mothers with syphilis had known they had the condition, they could have treated it during pregnancy to avoid passing it on to their children.
Instead, the condition caused 231 stillbirths and 51 infant deaths in 2022.
Dr. Danielle Ely, co-author of the report, told ABC News: “So what we’re seeing is that what we expected to be just a one-year gap is now a two-year higher rate.”
In 2022, rates of seasonal viruses like flu and RSV have rebounded after flattening during quarantine; both can be deadly to a newborn’s fragile immune system.
Dr. Eric Eichenwald, a Philadelphia neonatologist, he told PBS this increase was “concerning” and he blamed viruses for the increase. It is possible that the 2023 rate simply represents the continuation of this trend.
Additionally, demographer Amanda Jean Stevenson, who was not involved in the research, placed blame on a lack of standardized national care.
doctor stevenson told CNN: “We can certainly expect that maternal complications overall are increasing because standards of care for pregnancy-related complications are not being met in many states.”
Although this rate remained the same nationally between 2022 and 2023, in some states, such as Nevada and Washington, the rate of newborn deaths actually increased, by 31 percent and 16 percent, respectively.
In Mississippi, in 2023, there were 34,459 live births and 308 deaths, that is, for every 1,000 births, there were approximately 8.94 deaths.
Similarly, in Arkansas there were 35,264 and 290 deaths, representing 8.22 deaths per 1,000 births.
In Ohio there were 126,896 births and 909 deaths, which is 7.16 deaths per 1,000 births.
The graph above shows the infant mortality rate by ethnic group in 2021 (blue) and 2022 (green).
According to the American Journal of Managed Care, in 2022, the United States has the highest infant mortality rate than similarly developed countries, including Australia, Canada, France, Germany and Japan.
In the UK, 3.9 deaths per 1,000 births result in an infant death and in Australia, 3.2 deaths per 1,000 births.
Dr. Sandy Chung, president of the American Academy of Pediatrics, he told CNN: “We live in a country with significant resources, so the infant mortality rate and its increase are surprisingly high.”
He National Vital Statistics SystemThe arm of the CDC that publishes this report collected data from birth certificates, researchers classified them by race, sex, state of residence, and ten leading causes of infant death.
Maternal illnesses included conditions such as preeclampsia, dangerously high blood pressure that affects about 9.5 percent of pregnancies.
Black children remained more likely to die than any other group, closely followed by Native Americans and Native Hawaiians or other Pacific Islanders.
In addition to measuring the overall rates for each state, there were some states whose infant mortality rate worsened throughout the year.
Although Nevada and Washington saw the largest increases, rates also increased in states such as Rhode Island, Alabama and Kentucky.
Experts from the National Bureau of Economic Research He said this gap between the United States and other countries is largely due to two factors.
First, in Europe doctors are more likely to count babies born after 24 weeks as miscarriages, while in the United States they are more likely to count them as live births.
Second, babies in the United States are more likely to be born premature or with low birth weight. Both of these factors can increase a baby’s chance of dying.
Beyond national statistics, Dr. Chung said differences in health care from state to state, based on both the number of doctors and the type of public insurance available, may be contributing to the differences.

The United States regularly outperforms other developed nations in terms of infant mortality.
In some states, women have to drive for hours to get to the doctor, meaning they can skip pregnancy checkups and not even make it to the hospital to give birth.
In Mississippi, for example, a 2023 report found that half of women live in a county without access to maternity care. 24 percent of women did not have a birth hospital within 30 minutes of their home.
Dr. Chung said, “We know that for people living in or near poverty and for certain racial and ethnic groups there are significant challenges in accessing a doctor or receiving treatments.”
Additionally, research has shown that states that expand Medicaid coverage to cover mothers in the year after childbirth reduce the number of infant deaths. This is largely because uninsured women are more likely to skip doctor visits after giving birth than women who are covered by a plan.
Since then, many states have taken steps to adopt this plan. Arkansas, which is in the top five for the worst infant mortality rates, did not.
Dr Chung said: “We need to change policies to help families escape poverty and help them access health care before it is too late.”