Oncologists increasingly consider oral sex as the main driver of the steady rise in throat cancers.
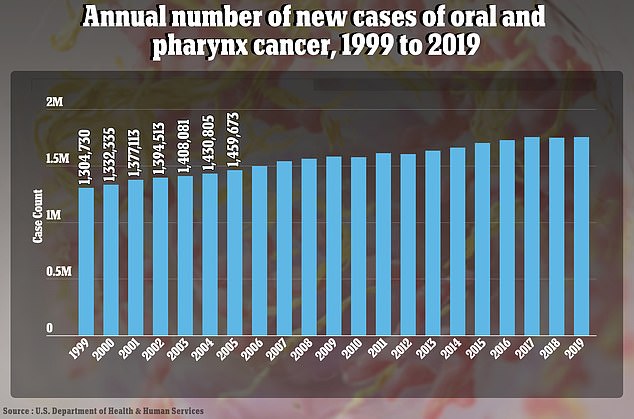
Rates of the disease have increased at a slow but steady rate of about one percent annually since the mid-2000s.
And while it tends to be more common in older adults, oropharyngeal cancer is increasingly diagnosed in younger people due to rising rates of human papillomavirus.
Dr. Hisham Mehanna, an oncologist at the University of Birmingham in the United Kingdom, wrote in the Conversation that the number of sexual partners throughout life, especially oral sex, is the main risk factor for this specific type of throat cancer.
People who have oral sex with at least one in six people with HPV in their lifetime are 8.5 times more likely to develop cancer of the throat, cervix, or genitals compared to those who do not have oral sex.
This graph shows how the number of new cases of throat cancer has increased in the US since 1999. It is increasing about one percent a year in women and three percent in men.
Research shows that more than 80 percent of men and women engage in oral sex, and surveys suggest those rates are increasing particularly among womenfrom 85 percent who reported oral sex from 2011 to 2013 to 89 percent from 2017 to 2019.
Most throat cancers (about 70 percent) are caused by human papillomavirus (HPV), a set of common sexually transmitted viruses that usually cause no symptoms and resolve on their own.
There is a very effective vaccine against HPV, but rates are considerably lower than the 85 percent needed to reach “herd immunity,” a term that means that enough people have become immune so that the virus cannot spread.
Less than 60 percent of schoolchildren have received the HPV vaccine for a variety of reasons, including parental hesitancy and anti-vaccine sentiment.
HPV strain 16 is strongly linked to mouth and throat cancers. In recent years, the incidence of these HPV-related cancers has increased significantly, largely due to changes in sexual behaviors, including more frequent practice of oral sex, according to Health Henry Ford.
Dr Mehanna appealed to parents around the world to vaccinate their children as the shots are very effective.
He said vaccines work “only if coverage among girls is high, above 85 percent,” and only if one remains within the covered “flock.”
“It certainly does not provide protection in countries where vaccination coverage of girls is low, for example the United States, where only 54.3 percent of adolescents aged 13 to 15 had received two or three doses of vaccine against the HPV in 2020”.
He added that the coronavirus pandemic has introduced additional difficulties.
On the one hand, schools were inaccessible for a time, making it difficult for young people to access. Additionally, growing vaccine hesitancy or “anti-vaccine” sentiment in several countries may be contributing to lower vaccination rates.
At the same time, condom use among young people is at historic lows.
An independent sample of men and women ages 15 to 44 was conducted from 2011 to 2015 to show condom use in relation to gender, age, race, and educational level.
When participants were asked about their last sexual experience, only 33.7 percent of men and 23.8 percent of women used a condom.
The survey was the first to cover Americans’ problems with condoms during sex, from some who said they “fell off completely” to others who only use them during part of the act.
More than 58,000 Americans were diagnosed with oral or pharyngeal cancer in 2024.

Those who have six or more oral sex partners in their lifetime are 8.5 times more likely to develop oropharyngeal cancer than those who do not practice oral sex.
While 69 percent of people diagnosed survive more than five years after diagnosis, the United States recorded 12,230 deaths this year.
Meanwhile, about one in four Americans has HPV, although most don’t know it due to a lack of symptoms. This can be dangerous because more than 11,000 women with HPV develop cervical cancer.
When a person receiving oral sex has HPV, they can transmit it to the person performing it.
When the virus enters the body through the throat, it lodges in deep crevices.
It disrupts the cell life cycle and cell death in the throat wall, causing some cells to grow uncontrollably.
This can lead to the formation of cancer cells that continue to accumulate until they cause a tumor.
It usually takes years for the virus to develop into throat cancer.
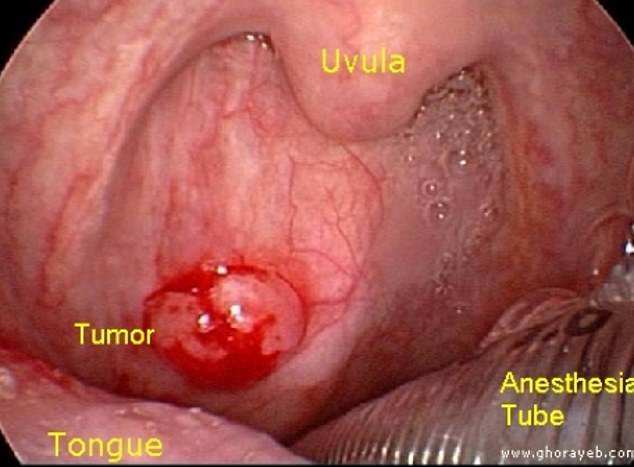
HPV causes about 60 percent of oropharyngeal cancers. Photo courtesy of medbullets.com
About 10 percent of men have oral HPV and 3.6 percent of women, mostly elderly.
Most people with HPV do not develop symptoms and the immune system usually clears them within a few years. But people with some type of defect in their immunity are more likely to develop genital or oral warts or cervical and genital cancers.
An HPV vaccine was introduced in 2006 for 11-year-olds, although initially for girls. It was approved for children in 2020.
While some adverse reactions have been reported, such as fever, fatigue and headache, 96 percent of these effects were not considered serious and the benefits of the injection have been shown to far outweigh the risks.
The HPV vaccination rate is relatively low, around 60 percent of adolescent girls, compared to other developed countries such as the United Kingdom, where 85 percent of adolescent girls have been vaccinated.
Unlike the United States, the United Kingdom government offers a universal HPV vaccination program, which is free for eighth graders, which is helping the country get closer to eliminating cervical cancer. .
Getting vaccinated as a teenager is equally crucial for preventing oropharyngeal cancer, as HPV has been shown to cause 60 to 70 percent of cases.