Weight-loss injections could help obese patients suffer fewer complications after surgery, new research suggested.
Injections like Ozempic and Wegovy, hailed by the likes of Elon Musk and Jeremy Clarkson, have been shown to help overweight people lose up to five pounds.
Now, according to experts, combining the treatments could be the most effective way to lose weight quickly before surgery.
US scientists said obese people who may be considered too high risk for bariatric (weight loss) surgery could qualify after taking the drugs.
Research shows that obese patients (with a body mass index (BMI) of 30 or more) are more likely to develop Surgical and anesthetic complications.
For these individuals, losing between five and ten per cent of their weight could reduce some of the risks, NHS sources say.
Now, according to experts, combining the treatments could be the most effective way to lose weight quickly before surgery. American scientists said obese people who may be considered “too sick” for bariatric surgery could qualify after taking the drugs. Research has long shown that patients with extreme obesity (a body mass index (BMI) greater than 70) face a higher risk of complications after surgery.
Dr. Phil Schauer, co-author of the study and director of the Metamor Metabolic Institute at Pennington Biomedical in Louisiana, said: “Combining anti-obesity medications can achieve much greater pre-surgery weight loss than other methods for people with obesity. extreme.”
“Many patients who would otherwise be considered ‘too sick for surgery’ may now qualify.”
According to the study, presented today at the 2024 Annual Scientific Meeting of the American Society for Metabolic and Bariatric Surgery (ASMBS), 113 people with a BMI greater than 70 attempted to lose weight before metabolic and bariatric surgery.
The researchers did not reveal the average age or sex of the participants or lifestyle factors such as smoking history and diet.
One group was given a combination of weight-loss injections, while another was offered a single treatment.
The third group received a doctor-supervised diet and exercise plan.
After a follow-up of 73 days on average, the scientists found that participants taking multiple medications experienced the highest percentage of total body weight loss (13.1 percent).
They were followed by those who received a single weight loss attempt (8.14 percent).
In comparison, volunteers who followed the diet and exercise plan experienced a 5.95 percent reduction.
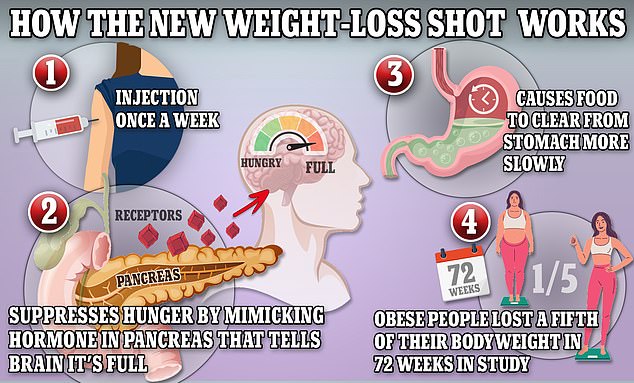
Weight loss medications like Ozempic and Wegovy mimic the production of the hormone GLP-1, which helps keep the body full.
The scientists also said that reductions in BMI were greatest six to 12 months later among those treated with a combination of treatments.
Obesity itself increases a person’s chances of suffering from serious health problems that can damage the heart, such as high blood pressure, as well as cancer.
Around two in three adults in the UK are obese or overweight, giving the country one of the highest obesity rates in Europe.
Last month, a sobering report also suggested that rising levels of obesity in Britain have fueled a staggering 39 per cent rise in type 2 diabetes among people under 40, with 168,000 Britons now living with the disease.
Weight gain has also been linked to at least 13 types of cancer and is the second leading cause of the disease in the UK, according to Cancer Research UK.
However, experts today cautioned that more research is first needed before recommending weight-loss injections to obese patients before surgery.
Dr Marina Kurian, president of the ASMBS, who was not involved in the research, said: “Further studies are needed to determine the optimal role of GLP-1 before and after bariatric and metabolic surgery among different patient groups.
“Obesity should be considered like other chronic diseases in which sometimes more than one therapy is necessary over time and for different reasons.”
Semaglutide, sold as Ozempic and Wegovy, and tirzepatide (Mounjaro) have been hailed as a monumental advance in the war against obesity.
The pens, taken once a day, mimic a hormone called GLP-1 and trick the brain and body into thinking they are full, curbing appetite.
Trials show that semaglutide, made by the Danish company Novo Nordisk, helps users lose up to 33 pounds (15.3 kg) on average in about a year.
Side effects from the injections, such as bloating, nausea and acid reflux, have long been noted by the government’s National Institute for Health and Care Excellence (NICE).
An increasing number of Ozempic users on social media have also complained of gaunt facial features, sagging “melted candle” skin, “empty” breasts and hair loss, which are not believed to be a direct side effect. of the medication but a consequence. spectacular weight loss.
Analysis suggests the cost of tackling the knock-on effects of the jabs on the NHS could rise to more than £100m a year.
Others, meanwhile, have warned about bad breath and even sexual dysfunction.
The latest NHS data shows that 26 per cent of adults in England are obese and a further 38 per cent are overweight but not obese.
Experts have pointed to a lack of exercise and poor diets high in ultra-processed foods as key factors in the UK’s obesity epidemic.
Wegovy was approved by the NHS last year, specifically for weight loss.
But the eligibility criteria for people who want to get the drug on the NHS (for the standard prescription price of £9.90 in England) are strict.
Mounjaro was received the green light from NICE to National Health Service Use in September for patients with type 2 diabetes who do not have the condition under control.
Health services do not yet use it for obesity.
But in February it became available privately in Britain, with clinics charging around £40 for a week’s supply.

