Food safety officials are searching for a mystery food that triggered an E. coli outbreak that killed 113 people and left at least 37 in the hospital.
Experts say the rare Shiga toxigenic variant (STEC) of the bug that causes diarrhea is “particularly unpleasant” and issued a warning to handle and cook food hygienically.
The source has not yet been discovered, but there are fears that the impending barbecue season, when many foods are not cooked sufficiently, could fuel an even larger outbreak.
The UK Health Security Agency (UKHSA) said it believes the cases are linked to a “nationally distributed food” or “multiple foods” and says it is investigating the cause.
Authorities have not yet traced the origin of the outbreak of Shiga toxin-producing E. coli (STEC), a rare strain of the virus that causes diarrhea. But they believe it is related to a “nationally distributed food” or “multiple foods.”
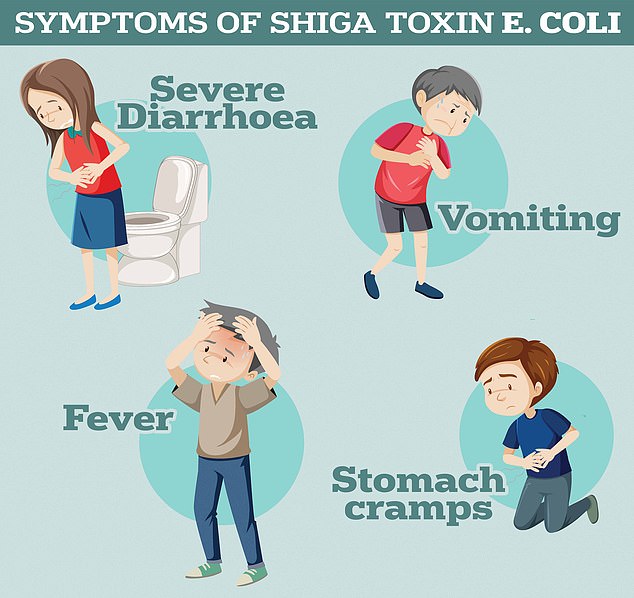
Symptoms of Shiga toxin-producing E. coli include severe diarrhea and vomiting, according to the UK Health Safety Agency.
Two-thirds of people known to have been infected by the bacteria became so seriously ill that they needed hospital care.
The victims include children as young as two years old, although the majority are young adults, according to UK health and food watchdogs.
UKHSA said a total of 113 cases were recorded between May 25 and June 4.
Of these, 81 were in England, 18 in Wales and 13 in Scotland.
Only one case has been recorded in Northern Ireland, although authorities say this individual probably contracted the virus in England.
Almost two-thirds (61 per cent) of cases in England became so sick they needed to be hospitalised.
STEC is primarily spread by eating contaminated foods, such as raw vegetables that have not been washed or stored properly or undercooked meat.
It can also be transmitted by touching infected animals or their feces, either directly or through contaminated water, and by coming into contact with other people who are sick and then touching your face and mouth without properly washing your hands.
But UKHSA said current evidence points to a food origin of the current outbreak.
“The source of this outbreak is not yet confirmed, but there is currently no evidence linking the outbreak to open farms, drinking water or swimming in contaminated seas, lakes or rivers,” he said.
However, the agency expects cases to continue rising as more testing is done.
Professor Nicola Holden, bacteriologist and member of Applied Microbiology International’s Food Safety Advisory Group, said: ‘STEC has been with us since the 1980s.
‘It is a bacteria in continuous evolution that, as a group, has a high degree of genetic diversity.
“Sometimes that makes it difficult to detect pathogens in surveillance efforts that may have the potential to cause disease, because their genetics don’t always follow a predictable pattern that definitively identifies them as such.”
STEC is considered extremely contagious; It only takes ingesting a few bacteria for a person to get sick.
Symptoms of infection include vomiting, fever, stomach cramps and diarrhea that can last up to two weeks.
But in up to 15 percent of cases, the virus can cause hemolytic uremic syndrome (HUS), a life-threatening condition that can lead to kidney failure.
Children under five years of age are at highest risk for HUS.
However, it can also affect other vulnerable groups, including the elderly and the immunocompromised.
UKHSA Incident Manager Trish Mannes urged Brits to take steps to avoid contracting or potentially passing on the infection to others.
“Washing your hands with soap and warm water and using disinfectants to clean surfaces will help stop the spread of infection,” he said.
‘If you are unwell with diarrhea and vomiting, you should not prepare food for other people while you are unwell and avoid visiting people in hospitals or nursing homes to avoid transmitting the infection in these settings.
“Do not return to work, school, or daycare until 48 hours after your symptoms have disappeared.”
Britain’s food safety watchdog, the Food Standards Agency, is also helping the UKHSA to “identify the source of the disease”.
People have been advised to contact NHS 111 or their GP if they or their children show any symptoms of E. coli infection.
For children under five, these may include disinterest in breast or bottle feeding and signs of dehydration, such as less wet diapers.
Both adults and children are advised to call NHS 111 or their GP if they continue to vomit for two days or have diarrhea for a week.
Anyone suffering from bloody diarrhea or bleeding from the bottom should call NHS 111 or their GP immediately.

