A mother of seven is risking her life by going ahead with a life-threatening pregnancy despite calls from doctors to terminate it.
Alex Gooding, from Arizona, is currently 18 weeks pregnant with a baby she named Chloe.
But pregnancy is a Caesarean section ectopic pregnancy (CSEP), in which the embryo implants within a deep scar in the uterus.
Doctors have repeatedly urged Gooding to stop treatment, warning that there is a high risk to both her and the fetus, including infertility and death in the future.
They say pregnancy could cause serious internal bleeding by opening up the scar as the baby grows or if the placenta ruptures from implanting in the wrong place.
But Mrs Gooding, who is pro-life, has rejected the advice and says she will carry her pregnancy to term.
Alex Gooding (pictured above with her family) has divided the internet with her decision to go ahead with her ectopic pregnancy.
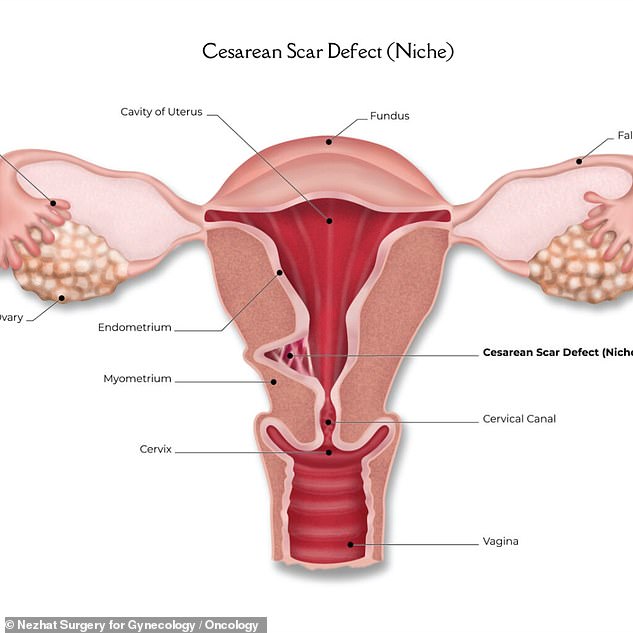
The above, of Nezhat Surgery in New York Cityshows what the uterus looks like if it has a scar from a cesarean section. In a CSEP, the embryo is implanted in the scar.
Mrs. Gooding is an Orthodox Christian and has lost six fetuses to miscarriages or complications.
She wrote on Instagram: ‘The general consensus among the medical field is to terminate these pregnancies due to the high morbidity and mortality for the mother.
“But there is a growing community of advocates for these CSEP babies to manage the pregnancy conservatively and hopefully make it to the side of the survivors (both mother and baby), which is the choice we have made.”
Ectopic pregnancies occur when fertilized eggs implant outside the uterus. There are several types of ectopic pregnancies, some of which implant in the ovary or fallopian tubes.
About one to two percent of all pregnancies in the United States are ectopic, and the fetus has “virtually no chance of survival,” doctors say.
CSEP is rare, occurring in about 0.05 percent of all pregnancies, according to 2019. studyalthough that number is increasing as more women have C-sections.
Doctors say these pregnancies generally do not differ from normal pregnancies in presentation, but they do carry a high risk of complications.
Among them is placenta accreta, when the placenta (a temporary organ that forms in the uterus and connects the mother and fetus) grows too deep into the uterine wall, which can cause heavy bleeding.
Another is placenta percreta, where the placenta grows through the uterine wall and fuses with other organs such as the bladder, requiring surgery to remove it.
The Society for Maternal-Fetal Medicine, which sets standards for maternal and infant health, recommends against continuing with a CSEP because of the risks.
But women can reject this advice, as long as health workers first inform them of the risk.
Gooding’s fetus is currently growing behind the placenta, according to her Instagram posts, and has a heart rate of 154 beats per minute, within the expected range at this stage of pregnancy.
Her page, which has more than 159,000 followers, has received an avalanche of negative comments about her decision to continue with the pregnancy.
One user wrote: ‘Your living children should come first. You are risking your life and the lives of your babies.’
A second said: “There is nothing pro-life about risking your life like this and leaving so many motherless children behind.”


Gooding is now revealing the progress of her pregnancy online, arguing that it is possible to carry her fetus to term.
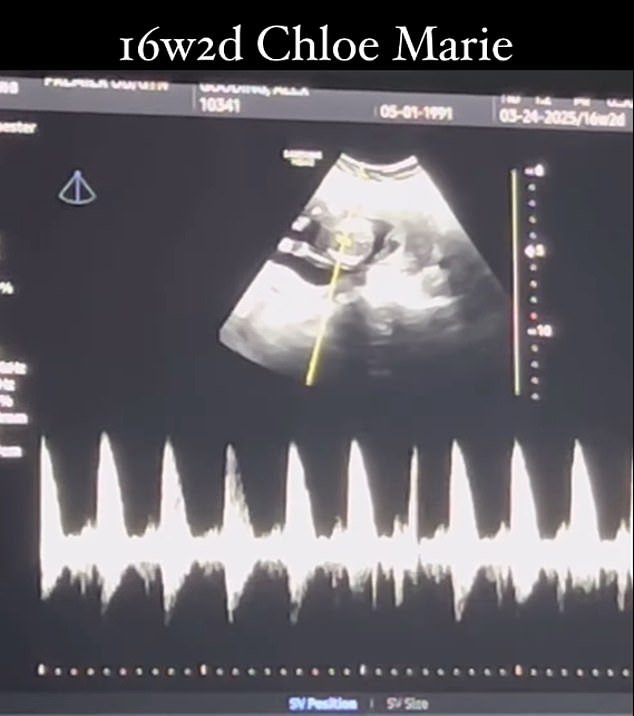
The above shows the fetus, which she named Chloe, in the womb.
A TikToker also posted about her, describing her decision to carry the pregnancy to term as selfish to her children.
But there has also been some support for his position online. Commenting on one of her posts, one user wrote: “I’m so proud of you for sticking to your beliefs.”
Another said, “I really believe God has favor with you for not killing your baby.”
Gooding discovered she had a CSEP five weeks into her pregnancy and quickly sought the advice of four doctors, who told her to terminate it.
She also said a doctor told her husband to convince her not to continue the pregnancy.
Mrs Gooding posted on Instagram: ‘The day we found out that Chloe implanted in my c-section scar and was therefore a c-section scar ectopic pregnancy, was very difficult.
‘The maternal-fetal medicine (specialist) I saw immediately after my first midwifery ultrasound told me I had to terminate the pregnancy.’
However, Mrs Gooding and her husband decided not to terminate the pregnancy and are continuing the pregnancy despite medical advice.
She posted: ‘Choose hope and choose life! Fighting for our sweet Chloe Marie every day at 18 (weeks) +3 (days) ectopic pregnancy with c-section scar.
“To anyone who continues to claim that there are no survivors for this type of ectopic, you are completely wrong and I am happy to prove it to you any day of the week.”
Despite her situation, the pregnancy has been normal so far, and Gooding said she suffered from morning sickness and gained about 15 pounds.
Ms. Gooding and her husband have suffered pregnancy losses in the past, losing six babies due to miscarriages or complications.
When asked about Mrs. Gooding’s case, Dr. Veronica Gillispie, a New Orleans obstetrician who has not seen Mrs. Gooding as a patient, said: “The recommendation of the Society for Maternal-Fetal Medicine is that she not recommend that pregnant women carry these pregnancies to term. due to the risk of serious morbidity.
‘That said, I believe in patient autonomy. If you have been adequately advised about the risks and benefits and understand them, then you have the right to continue with the pregnancy.
“It would just be the care team being prepared in case something unfortunately happened during the pregnancy, and in terms of considering the timing of delivery and all those things.”
There is little anecdotal evidence that shows that it is possible to carry out a PESE.
in one study at King’s College LondonIn the United Kingdom, researchers followed ten women who underwent CSEP and all were diagnosed before the 12th week of gestation.
None of the mothers died and all gave birth to babies between 26 and 38 weeks. (This is just below the average of 40 weeks. A fetus can be viable outside the womb as early as 24 weeks.)
But half of the women had to have their uterus removed due to haemorrhage, while two also had a premature birth after the gestational sac, containing the fetus, protruded from the uterus.
Gooding has acknowledged the risks but has chosen to “conservatively manage” her pregnancy.
She wrote: ‘CFSPs carry high morbidity and high mortality for the mother and baby.
‘Most women who choose to continue carrying their babies experience CSEP (many of these). This is in no way downplaying the risk. These are real complications that many face in this type of ectopic pregnancy.
“We have chosen to manage my CSEP conservatively with Chloe and give her and I the opportunity to come out alive on the other side after seeing a second (maternal-fetal medicine specialist).”

