They are a surprisingly deadly health problem that can kill half of those who suffer from it within five years, according to studies.
Bone fractures, especially hip fractures, are said to be more deadly than cancer in people over 65.
The common problem has long been linked to increased mortality due to its impact on independence and movement in old age.
Now, a simple five-minute questionnaire could quickly reduce the chances of suffering a life-threatening fracture by identifying those at risk.
Experts say fractures can be prevented by avoiding the development of osteoporosis, a bone-weakening disease, through strengthening exercises and dietary changes, as well as increasing vitamin D levels.
More than 14,000 women at risk of fractures following a decline in bone density during menopause may now benefit from a new osteoporosis drug.
He toolDeveloped by the Global Osteoporosis Foundation, it asks questions about medical history, previous bone problems and exercise habits, and uses this to calculate the likelihood of developing the disease.
A low score indicates low bone density and therefore a high risk of osteoporosis, while a higher score suggests that the bones are healthy.
Those with a low score are advised to seek further testing from their GP, who may recommend lifestyle changes or prescribe medications such as romosozumab, teriparatide and alendronic acid to reduce fracture risks.
This comes shortly after the National Health and Care Excellence (NICE) watchdog approved a new drug called abaloparatide for 14,000 women at risk of fractures.
Dr Taher Mahmud, consultant rheumatologist at the London Osteoporosis Clinic, says the drug “can play an important role in rapidly reducing fracture risk” but warns it should be secondary to major lifestyle changes.
According to NICE, more than two million women in England and Wales suffer from osteoporosis. The disease, which develops slowly over several years, causes weak bones, which increases the likelihood of fractures, according to the NHS.
According to NICE, more than 2 million women in England and Wales suffer from osteoporosis, a bone-weakening disease.
According to the Global Osteoporosis Foundation, women are four times more likely to develop osteoporosis than men.
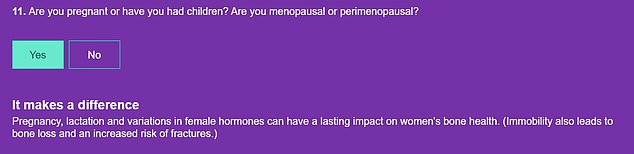
Lower bone mass, longer life expectancy and hormonal changes during pregnancy and menopause are some of the reasons for this.
The disease, which develops slowly over several years, causes bones to weaken, making them more likely to break, the NHS says.
For many, a broken bone is the first sign of the disease, but it is sometimes detected in older people by a particular posture or by pain during daily activities.
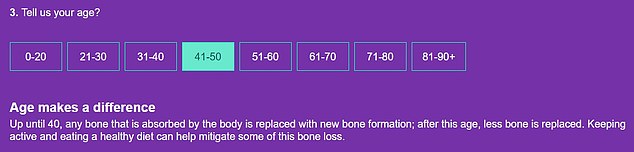
The 14-question questionnaire asks you about your age, sex, height and weight and whether your height has decreased in recent years.
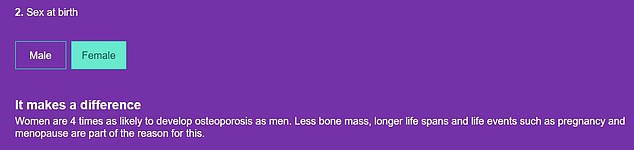
Women are four times more likely to develop osteoporosis than men, the authors of the questionnaire warn. Lower bone mass, longer life expectancy and life events such as pregnancy and menopause are some of the reasons for this situation.
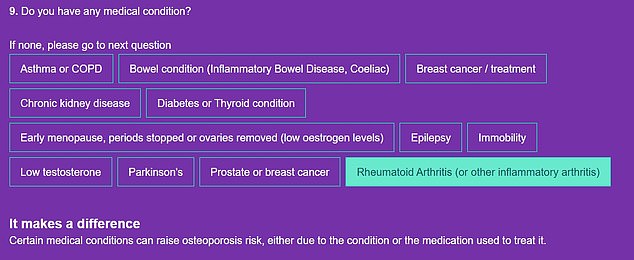
He or she will also ask about your medical history, including whether you have had any fractures, whether you take steroids, and whether you have any long-term health conditions such as breast cancer or rheumatoid arthritis.
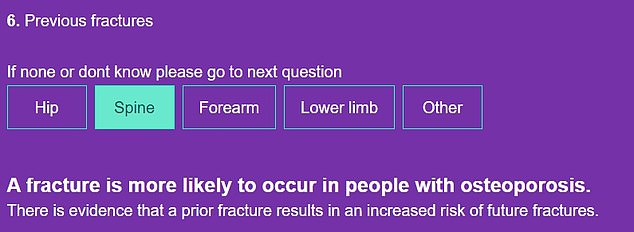
One question on the questionnaire asks if you have ever broken a bone, this is because previous fractures can increase your risk of future fractures.
The 14-question questionnaire asks you about your age, sex, height and weight and whether your height has decreased in recent years.
He or she also asks about your medical history and asks about fractures, steroid prescriptions, and long-term health problems like breast cancer or rheumatoid arthritis.
The survey asks if you drink, smoke, are pregnant or in menopause, and how much vitamin D you take.
The so-called “sunshine vitamin” is essential for helping bones absorb calcium, making them hard and strong.
Finally, it asks you what type of exercise you do each week.
In addition to menopause, taking steroids for more than three months or medications for anti-inflammatory conditions can also increase your risk.
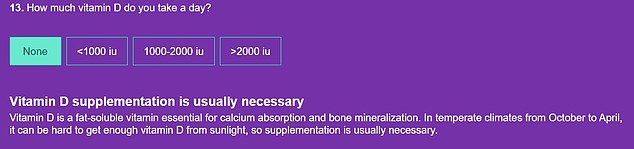
Not taking any vitamin D supplements is also considered a risk factor, as this vitamin is vital for calcium absorption.

Finally, it asks you what type of exercise you do each week, choosing between walking, swimming, running, HIIT, weight training and cycling.

The drug, called abaloparatide, is vital in helping bone density during menopause because estrogen, the hormone that is important for maintaining bone density and strength, decreases and bone density is reduced.
It then calculates a score from one to ten to determine the risk of osteoporosis and highlights factors that may increase the risk.
Those who score between nine and ten are simply told to maintain their bone health, while people with a score between six and eight are advised to discuss their result with their GP.
But people who score below five are advised to seek further evaluation.
In addition to menopause (when bone-stimulating estrogen levels decline), taking steroids for more than three months or medications for anti-inflammatory conditions can also increase your risk.
Other factors include having an eating disorder, having a low BMI, not exercising regularly, and excessive drinking and smoking.
Age is also a factor, as bone cells are replaced by the body up to age 40. But after that age, less bone is replaced, which means you’ll need to stay active and eat a healthy diet to mitigate some of this bone loss.
While Dr Mahmud believes the new osteoporosis drug abaloparatide “marks a significant advance in the treatment of bone health”, he cautions that medication should be secondary to major lifestyle changes.
He added: “While drugs like abaloparatide can increase bone density, they do not address underlying problems such as poor nutrition, sedentary lifestyle or hormonal imbalances.”
‘While we welcome new treatment options such as abaloparatide, our core message remains the same: the best approach to osteoporosis combines lifestyle changes, proper nutrition, targeted exercise and judicious use of medications when necessary.
“Our policy is to encourage all women to assess their bone health and take proactive steps to maintain strong bones throughout life,” she said.
‘Many people are only diagnosed with osteoporosis after they have suffered a fracture and we believe it should be identified earlier and, more importantly, prevented in the first place through patient education.’

