The body of an Alaskan mother of four who disappeared after jumping into a river to save her dog has been found, more than four months after she went missing.
The family of Amanda Richmond Rogers, 45, said KTUUU that officials recovered his body from the Eagle River on Sunday. His dog, Groot, was frozen in his arms.
Rogers, an emergency room and hospice nurse, went missing Dec. 23 after jumping into icy waters to rescue the dog after it fell through the ice.
The 45-year-old and her husband, Brian, a doctor, were taking a walk in the frozen desert on their 18th wedding anniversary.
Alaska State Troopers and the Alaska Dive Search and Rescue Team combed the waters for the mother of four, with the help of Alaska Solstice Search Dogs.

The remains of Amanda Richmond Rogers, 45, were recovered Sunday, more than four months after she disappeared in an icy river.


The Alaska woman was hiking with her husband, Brian, to celebrate their 18th wedding anniversary when their dog stopped to drink from the river and fell on the ice.


The mother-of-four started swimming down the river after her beloved pet went missing. They found her with her body in her arms.
“They told me any of them would have made the same decision to rescue one of their fur babies,” said sister Jennifer Richmond.
The desperate search came to an end Sunday, when Anchorage police were notified of the remains of a deceased person near the North Fork Trailhead.
Rogers’ body was pulled from the water and taken to the State Medical Examiner’s Office to determine the cause of death.
The discovery of his remains was another stab in the heart for the relatives who had already had to accept their loss months before.
While friends and loved ones awaited the news with bated breath, many had already accepted that they would never see her again.
“I miss you Amanda and I will always miss you,” Rogers’ aunt, Susie Harris, wrote on Facebook in January.
‘My beautiful niece who had a heart of gold and love for all things. We will miss her very much. Our hearts are broken.’
Marissa Painter learned of the discovery of her close friend’s remains on Wednesday. “Thank God they found her holding Groot,” she said.
In a previous social media post, Painter described having an “instant connection” with Amanda, whom he considered his “soul sister.” The couple first connected when Amanda wanted to adopt a Goldendoodle puppy.
“We kept in touch with pictures and messages, we checked on each other because we knew our family lives were busy with kids and homes, we talked about our families getting together in the summers for adventures,” Painter said.
‘We were supposed to go on a trip last summer, but her adventures led her to clear a trail, so we postponed it.
“Let me tell you, make those trips happen somehow because you never know when things will change and you’ll never be able to make them.”


Alaska State Troopers and the Alaska Dive Search Rescue and Recovery Team searched for Rogers with the help of Alaska Solstice Search Dogs.


Anchorage police were notified of the discovery of his remains on Sunday. His body was transferred to the State Forensic Medical Service to determine the cause of his death.


Rogers’ sister, Jennifer, expressed her gratitude to the Alaska Diving Search and Rescue Team for their tireless work to find the mother of four.


Brian, a doctor, explained how the pair lay down to rest in a scenic area while Groot tried to drink from an opening in the ice and fell.
Jennifer Rogers expressed her deep gratitude to the Alaska Diving Search and Rescue Team in late January for their efforts in finding her beloved sister Mandy.
“I have no words for your love, commitment and compassion,” he wrote.
‘Whether it’s for my sister or just love, you won’t find a more dedicated team. From the depths of our broken hearts, thank you.”
The mother-of-four’s husband of almost two decades wrote a moving tribute just days after she disappeared underwater, remembering the day his life changed forever.
He explained that he and Rogers were busy decorating the house and wrapping presents for Christmas. He marked the first holiday they had celebrated since the death of Rogers’ father earlier that year.
“After spending time with his mother and sister the previous two days, the 23rd was our day,” he said.
‘We got married on December 23, 2005, so this is our 18th anniversary. We planned to walk two of our dogs, go on a date, and spend the night at the Captain Cook Hotel. It was a beautiful day.’
He explained that the couple chose to hike the North Fork trailhead of the Eagle River, which was “one of Amanda’s favorites.”
Tired of walking through the snow, they stopped to rest in a picturesque area by the water.
When his dog Groot tried to drink from a small opening in the ice, “no more than 18 inches wide,” he fell. “Before you even think,” Brian jumped in after him.
‘I clung to the edge of the ice as I frantically crouched under the ice, reaching into the darkness trying to feel and grab our dog. I didn’t feel anything,’ he said.
When he ran out of breath and returned to shore, he turned around and saw Rogers wading into the water.
“I knew from the look on his face that he was going to save our dog,” she wrote. ‘She is an emergency nurse, trained to help and save people. In this situation, she was going to save our dog.’
Brian yelled at her and before he could restrain her, Rogers began swimming down the river under the ice and disappeared.
“To anyone wondering why we would jump in to save our dog, I can only answer that our instincts took over and we jumped in without thinking,” he said. ‘Amanda loved her dogs almost as much as our children, they were our family.
‘She didn’t jump in to save “just a dog”, she was a family member. “To me and our four children, she died a hero.”


He detailed Rogers’ love of dogs, writing, “To me and our four children, she died a hero.”
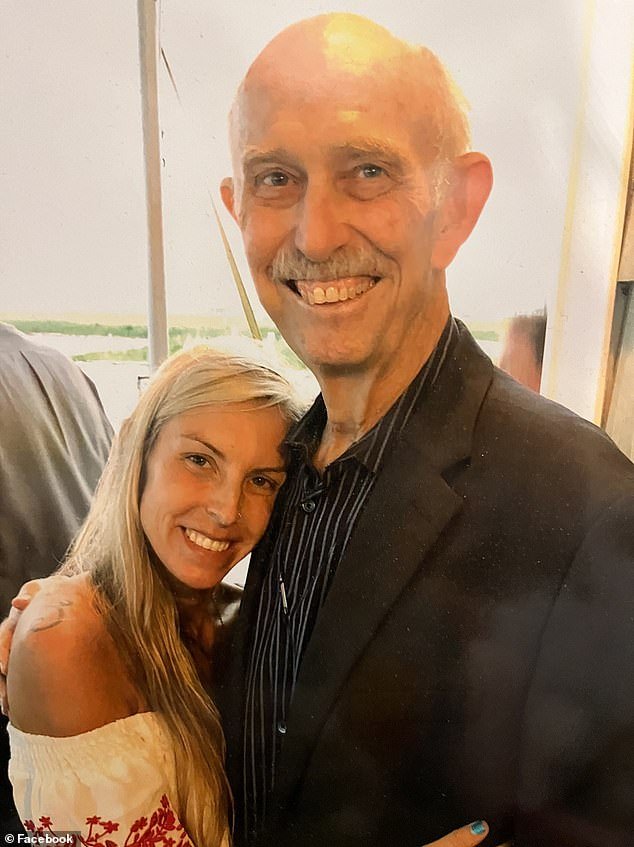
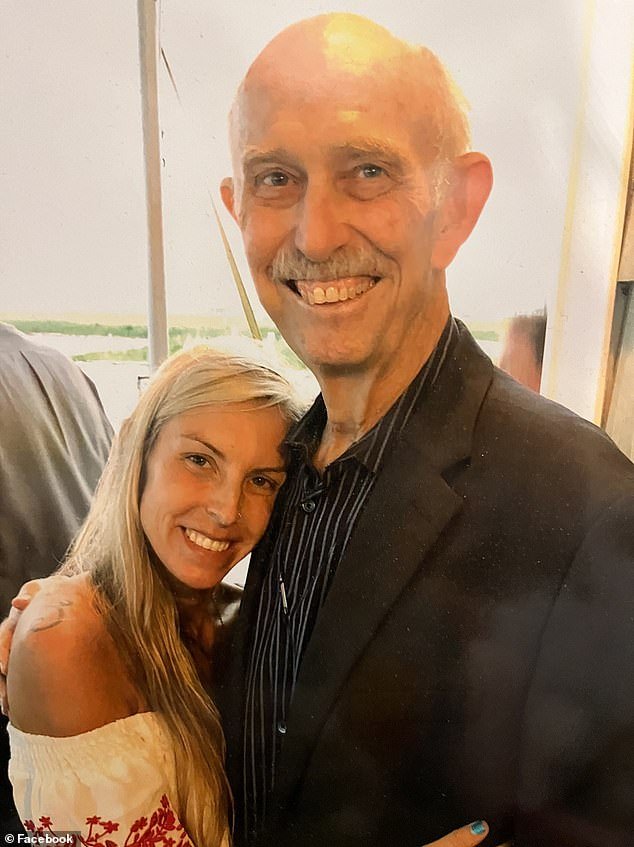
Rogers (pictured with her late father) was honored at a memorial ceremony in March, where she was officially relieved of her nursing duties.
He described his beloved wife as “an incredible mother” of “four tremendous children.”
“She worked as an emergency room nurse, death scene investigator and pediatric palliative care nurse, but the job she excelled at was being a mom,” Brian said.
‘She enjoyed the outdoors, her family, all the animals and adventure. She has improved the lives of many people. She could go on and on and on. She was a beautiful person with a beautiful soul.’
Crowds packed the Eagle River High School gym in March to honor the loving mother of four.
Registered nurse Christine Dittrich rang a triangle as part of the Nightingale Tribute, a ceremony used to honor a fallen nurse. “We officially released her from her nursing duties,” she said.
Rogers’ four children also spoke during the funeral.
“Mom was such a unique and special person that God couldn’t wait any longer to see her in heaven, and I don’t blame him,” said 17-year-old Liam.
Ten-year-old Bodhi recalled how his mother “would prefer dad and his kids and his dogs over anything in the world.”
On August 15, he said the ceremony would “make you cry because we won’t be looking at how much time we don’t spend with her, but all the time we do.”
Rogers’ eldest son, Leif Thurmond, 24, encouraged attendees to follow in his footsteps “and leave this earth without regrets.”
A memorial fund has been created in Rogers’ name to Alaska Dive Search Rescue and Recovery Team as well as Alaska Solstice Search Dogs.