Britons could be just over a year away from receiving a “game-changing” jab in the NHS to treat one of the deadliest forms of skin cancer.
Early results from the treatment, developed by pharmaceutical giants Moderna and MSD, found that it dramatically improved the chances of melanoma survival and could stop the cancer from coming back.
Now University College London Hospitals NHS Foundation Trust (UCLH) is leading the final phase of trials of the personalized mRNA vaccine, which scientists hope can also be used to stop lung, bladder and kidney cancer.
So how does it work? When will it be available? And could the treatment be used to treat other types of cancers?
Here MailOnline explains everything you need to know about the therapy.
What are mRNA vaccines?
While the science dates back to 2005, the first vaccines to use mRNA technology were those manufactured by BioNTech and Moderna against the Covid virus.
Messenger RNA, or mRNA, is a genetic blueprint that tells cells to make proteins in the body.
Unlike other traditional vaccines, a live or attenuated virus is not injected nor is it necessary at any time.
For Covid, the mRNA vaccine instructed cells to produce the spike protein found on the surface of the virus itself.
These harmless proteins “train” the immune system to recognize the virus and then produce cells that fight it if someone later becomes infected with the real virus.
How does melanoma treatment work?
Known as mRNA-4157 (V940), the injection activates the immune system to fight the patient’s specific type of cancer and tumor.
To create the treatment, a sample of the tumor is removed during the patient’s surgery.
DNA sequencing is then carried out to identify proteins produced by cancer cells, known as neoantigens, which will trigger an immune response.
They are then used to create a personalized mRNA vaccine that tells the patient’s body to generate tumor-specific neoantigen proteins.
Once injected, the immune system reacts to the proteins by creating T-fighter cells that attack the tumor, killing cancer cells.
The immune system should recognize any future rogue cells, in the hope of stopping the cancer from coming back.
What have the trials shown?
Scientists have given trial participants the vaccine along with an immunotherapy drug, pembrolizumab or Keytruda, which also helps the immune system destroy cancer cells.
Phase 2 trial data released in December found that people with severe, high-risk melanomas who received the vaccine along with Keytruda were almost half (49 percent) as likely to die or have their cancer return after three years than those who received Keytruda alone.
Patients received one milligram of the mRNA vaccine every three weeks for up to nine doses and 200 milligrams of Keytruda every three weeks (for a maximum of 18 doses) for about a year.
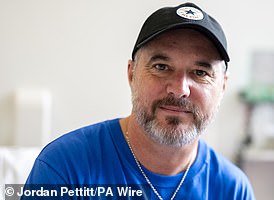
Dr Heather Shaw, national coordinating investigator for the UCLH trial, said there were real hopes the therapy could be a “game changer”, particularly as it appeared to have “relatively tolerable side effects”.
These included tiredness and soreness in the arm when the injection was given, he said, adding that for most patients it seemed no worse than receiving the flu or Covid vaccine.
When will the vaccine be available?
The combination treatment is not yet routinely available on the NHS, outside of clinical trials.
But Stéphane Bancel, CEO of Moderna, believes an mRNA vaccine against melanoma could be available in 2025.
The global phase three trial will include a broader range of patients and researchers hope to recruit around 1,100 people.
At least 60 to 70 patients will be recruited across eight UK centers including London, Manchester, Edinburgh and Leeds.
The twin therapy combination will also be tested in lung, bladder and kidney cancer.
Patients in the trial must have had their high-risk melanoma surgically removed within the last 12 weeks to ensure the best outcome.

Dr. Heather Shaw, the trial’s national coordinating investigator, described it as “one of the most exciting things we’ve seen in a long time.”
Why is melanoma so deadly?
The disease occurs after the DNA of skin cells is damaged, triggering mutations that become cancerous.
Melanoma begins in cells called melanocytes. These produce the pigment melanin, which gives color to the skin.
Around 15,000 Britons and 100,000 Americans are diagnosed with melanoma each year. It is the fifth most common cancer in the UK.
The incidence in Britain has risen faster than any other common cancer.
The increase has been attributed to increased exposure to UV rays from the sun or tanning beds.
Despite enormous advances in treatment, which have seen survival rise from less than 50 percent to more than 90 percent in the last decade, it still kills more than 2,000 people a year.
Melanoma usually grows quickly and can quickly pass through the skin and reach the blood vessels underneath. Once cancer cells enter the bloodstream, the disease can spread throughout the body.
Patients with melanoma are offered surgery, especially if it is caught early. Radiation therapy, immunotherapy drugs, and chemotherapy are also used.
Could the injections work for other types of cancers?
All the big pharmaceutical companies are competing to produce successful cancer vaccines. Last May, BioNTech, in collaboration with Roche, proposed a Phase 1 clinical trial of a vaccine targeting pancreatic cancer.
The following month, at the American Society of Clinical Oncology conference, Transgene presented its findings on its ENT viral vector vaccines. [ears, nose and throat] and papillomavirus-related cancers.
And in September, Ose Immunotherapeutics made headlines with its vaccine for advanced lung cancer.