The world was captivated by the royal wedding of Prince Andrew and Sarah Ferguson in 1986.
But what was once described as a fairytale romance between fiery redhead Sarah and the man of her dreams would ultimately end in heartbreak.
The couple first met when Princess Diana invited Sarah to a dinner at Windsor Castle and sat her next to the prince.
A whirlwind romance ensued and the two married at Westminster Abbey on July 23.
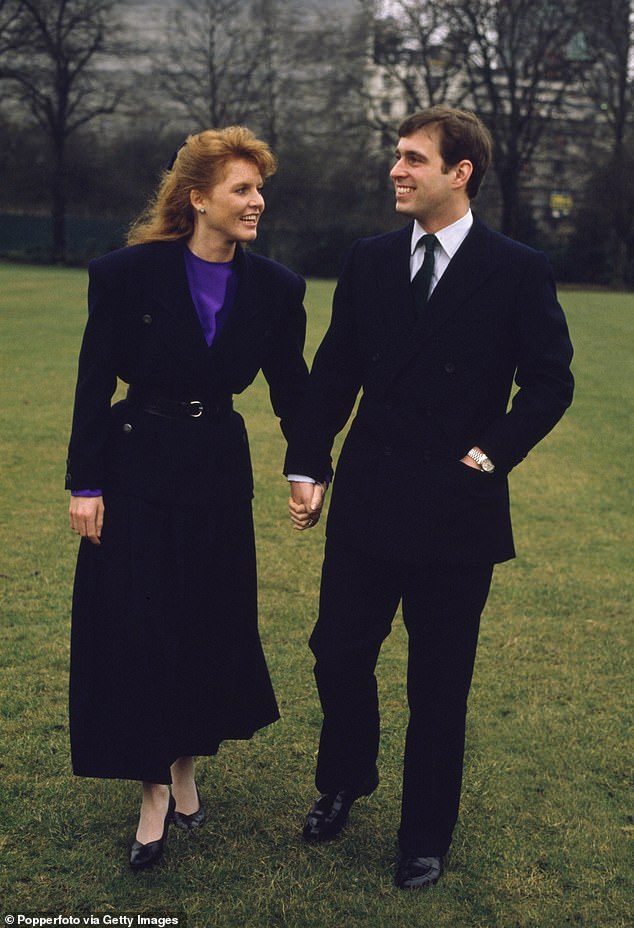
Prince Andrew and his fiancée Sarah Ferguson inside Buckingham Palace after announcing their engagement in March 1986


Sarah and Prince Andrew on the balcony of Buckingham Palace on their wedding day in July 1986
At the time, Sarah had only one request: that they could always be together.
But Andrew, a serving naval officer, was sent back to sea just two weeks after their wedding.
It is believed that cracks began to appear early in their relationship.
Fergie revealed they only saw each other 40 days a year during the first five years of their marriage.
“I spent my whole first pregnancy alone,” Sarah later told Harper’s Bazaar of Andrew’s absence. “When Beatrice was born, Andrew was given 10 days of shore leave. »
In early 1992, the couple legally separated. However, they continued to present a united front with their daughters, pictured together at the Royal Windsor Horse Show a few days later.
In August of the same year, the situation became complicated. Sarah was pictured on holiday in Saint-Tropez with her financial advisor John Bryan.
As the pair holidayed together, intimate photos were taken of the American businessman appearing to kiss the topless duchess’ toes.
When the news broke, Fergie was on a summer holiday at Balmoral Castle with the Queen, Prince Philip and Prince Andrew.
Queen Elizabeth was said to be mortified and Fergie’s relationship with her father-in-law Prince Philip was ruined forever.
The Daily Mail later wrote that Philip no longer even wanted to be in the same room as Sarah, insisting she had “shamed” the whole family.
Their divorce was officially finalized four years later on May 30, 1996, but by then the Duchess was already estranged from the royal family after her scandal.


Andrew and Fergie with their two daughters, Princesses Beatrice and Eugenie, at the Royal Windsor Horse Show after their separation in 1992
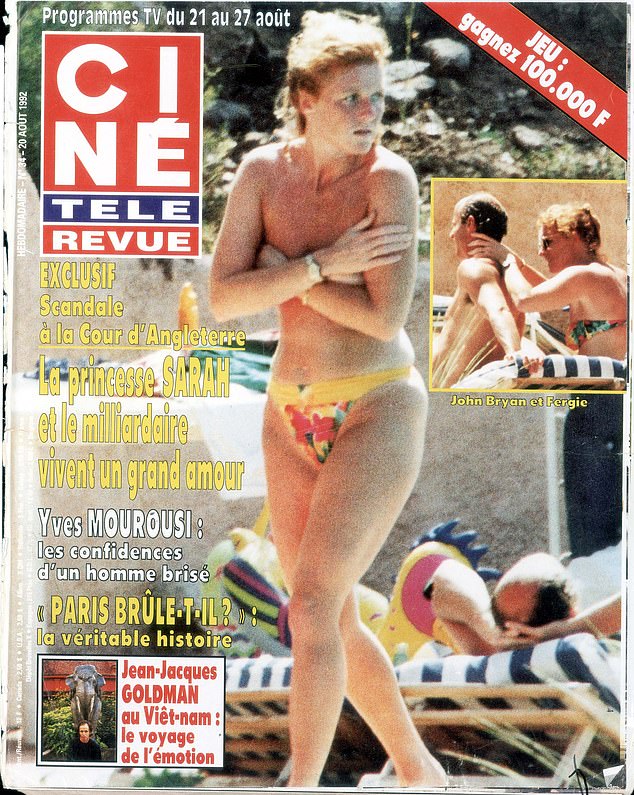
A few months after Andrew and Sarah split, Sarah was photographed in Saint-Tropez with her financial advisor John Bryan.
After the split, she told Harper’s Bazaar:
“I wanted to work; It’s not right for a princess of the royal house to be commercial, so Andrew and I decided to make the divorce official so I could go and find a job.
Some reports at the time suggested she was waiting for a larger divorce settlement.
Sarah, however, denied the claims, stating that all she wanted was to be on good terms with Andrew’s family again, especially the late Queen.
Even though nearly three decades have passed since their divorce, the Duke and Duchess have remained friends throughout the years.
They raised Princesses Beatrice and Eugenie together and Fergie continues to live in Prince Andrew’s home at the Royal Lodge in Windsor.
In fact, the two appear to be spending more time together than in their entire ten years of marriage.
And the couple regularly goes on vacation with their daughters.


The Duchess pictured escorting young Princess Beatrice to Windsor School after the Yorks’ separation was announced.


Prince Andrew pictured on the day the couple split, which was the same day as their engagement anniversary
Sarah previously told the Daily Mail: “We are the happiest divorced couple in the world. We are separate from each other, not from each other.
Speaking about their wedding day and their continued relationship, she added: “July 23, 1986 was the happiest day of my life. Andrew is the best man I know. What he is doing for Britain is incredible; no one knows how hard he works for his country.
“My duty is to him. I’m so proud of him. I am by his side and always will be. Our way of being is our fairy tale.
“Even though we’re not a couple, we really believe in each other. The Yorks are a close-knit family. We showed it.
