How much do you have in common with a mouse? The question is not as fatuous as it seems: mice are the animal most used in laboratory tests to find new treatments.
Chances are, every time you take a pill, apply an ointment, or get a vaccine, it will have been tested on a humble mouse.
The wisdom has always been that what is good for the mouse will probably be good for us humans, and it is better that the initial and potentially risky tests of new treatments be done in a laboratory animal than in a human.
And there is no doubt that the use of animals has advanced medical science.
It was thanks to work with dogs, for example, that the hormone insulin was identified for the first time in 1921, a great advance for people with diabetes and which has saved millions of lives.
Work with mice and monkeys led to the development of polio vaccines, which have helped prevent approximately 20 million cases of paralysis among children since 1988 alone.
Animals have also been key in testing semaglutide (the active ingredient in weight-loss injections Wegovy and Ozempic), and experiments in rodents confirm its potential for weight loss.
And much of our understanding of cancer and how it is treated has been supported by animal research.
“Without it we would not have discovered that cancer is not a disease, but that there are more than 200 different types, and of 300 anti-cancer drugs, around 250 are the result of animal research,” says Chris Magee, policy director from Understanding Animal Research, an organization that aims to explain why animals are used in research.
According to Home Office figures, 2.68 million “scientific procedures” involving live animals were carried out in Britain in 2023.
While 95 percent of them used mice, fish, birds or rats, 1.2 percent used cats, dogs, horses and “non-human primates” (i.e. monkeys).
Most of the procedures involved “basic research” on the nervous system, immune system and cancer, but 45 percent involved breeding genetically altered animals for research.
The perceived wisdom has always been that what is good for the mouse will probably be good for us humans (stock image)
Animal lovers understandably wince and the question is: does it really help the progress of medical science?
In fact, some argue that animal testing sometimes delays the development of new treatments. This is because potential therapies that fail safety testing in animals could still work in humans.
The fact is that the immune system of a mouse, for example, only has 10 percent in common with ours.
“And our lifespan is much longer and our tissue repair mechanisms are very different, as we need to survive longer,” says Andrew Knight, veterinary professor of animal welfare at Murdoch University in Australia.
“Most animal research simply does not predict human outcomes reliably enough to be useful in human diseases.”
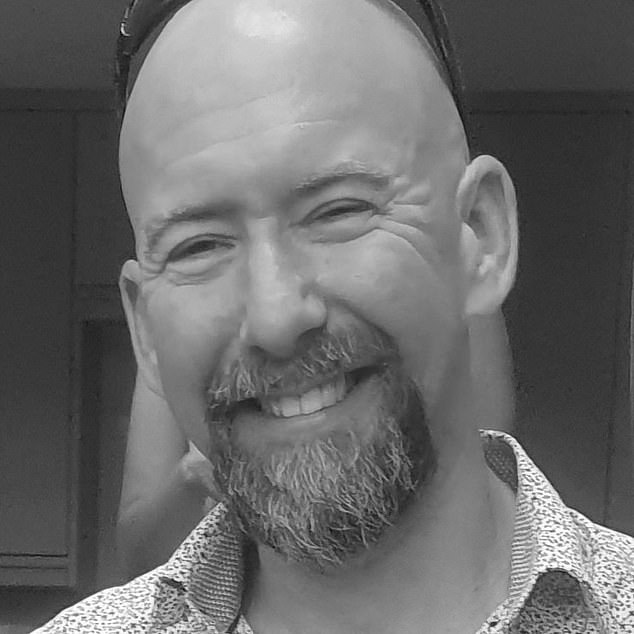
Chris Magee, head of policy at Understanding Animal Research, an organization that aims to explain why animals are used in testing.
Recent research from the University of Zurich found that only 5 percent of treatments that show promise are approved for use in humans. Researchers examined data from 367 potential treatments for 54 human diseases and found that, although half reached human testing, most failed.
One reason, they said, was that testing in “young, healthy animals…may not be directly applicable to the more complex scenarios of elderly patients with multiple health conditions.” Another was the “poor quality” of the animal studies.
While most scientists believe that animal testing remains a valuable tool, it remains controversial.
To develop a new drug, thousands of compounds are initially run through computer programs to identify potential candidates for a condition.
“Then you start testing on animal or human cells in the lab, and if there’s still hope, you move on to fruit flies,” says Magee, “but it takes years to get to this stage.”
After this other animals appear. Zebrafish are increasingly used because they are cheap, short-lived and, most importantly, transparent, Magee says. “So you can see what’s going on inside while they’re alive.”
Mice account for about 60 percent of animal research. “A major advantage is that its half-life expectancy is two years, which is useful if you want to see any long-term effects,” says Magee.
And about 90 percent of human genes are the same as those of a mouse and we have the same organs in similar places.
If something passes safety checks in the kidneys of mice, there is a 96 percent chance it will also pass in humans. In the cardiovascular system, the probability is 75 percent and in the gastrointestinal tract, 69 percent. But there are also important differences. Mice lack tonsils, their hearts beat faster, their cholesterol levels are significantly lower, and they break down fats differently.
That means wild mice don’t develop heart disease.
And using mice poses challenges for diseases like Alzheimer’s, since they do not develop the disease naturally.
Therefore, they have to be genetically modified to have an inherited form of the disease, says Dr Kamar Ameen-Ali, senior lecturer in biomedical sciences and dementia researcher at Teesside University.
The problem is that “less than 1 percent of people have this form of Alzheimer’s,” he says, and mouse tests don’t “really reflect the complexity of the disease as we see it in most people.”
Before a new drug is tested in humans, it will also be tested in another animal, such as a dog or rabbit.
This measure was introduced after the thalidomide scandal in the 1960s, when a drug women took for morning sickness caused limb deformities in their children. It did not cause limb deformities in mouse pups, but it did in later tests in rabbits.
However, even that is not certain. In 2006, six men almost died after being injected with a possible new drug for leukemia and autoimmune diseases at Northwick Park Hospital in Harrow. It had passed safety tests on several animals, including monkeys.
Shortly after receiving the TGN1412 drug, all of the young, healthy volunteers were in intensive care fighting for their lives.
The drug is thought to have caused an overreaction of the human immune system, but differences in the way genes activate immune cells meant this did not occur in animals.
“One argument in favor of animal testing is that we share many genes with mice, for example, but that doesn’t prove anything: we also have genes in common with bananas,” says Dr. Pandora Pound, research director at Safer. Medicines Trust. , a charity driving further development of human-based drugs.
«The important thing is not to have genes in common, but how the genes work, and in this respect there are great differences between us, mice and primates. And a small difference can be significant when it comes to testing a drug.”
The other problem is flaws in the way animal studies are designed.
Professor Knight says: “Often a problem with primate studies is that they include only two or three animals, but that won’t give a result that can be applied to a population.”
On top of that, he says, mice are nocturnal and the noisy lab environment during the day increases their stress levels, which can throw off the results.
“Temporarily, things like immunity and digestion become depressed,” says Professor Knight. ‘This works when the stress is short-lived, but when it is prolonged – as happens in these laboratories – the immune system is depressed for a long period of time,’ he explains. “So you take an animal that doesn’t predict human responses very well, and you further distort the immunological competence of that animal.”
What’s more, the difference in biological clock means that drugs tested in mice during the day, when they are biologically primed for sleep, may have a different impact on humans when administered at the same time, who will naturally be more alert.
In a study, published in 2020 in Nature, researchers at Massachusetts General Hospital found that three drugs used to treat stroke in mice reduced brain tissue death if administered during the day (when the mouse was biologically primed to sleep). , but they failed when administered. at night.
“There is a risk that we are throwing away safe and effective new drugs because of poorly designed research,” says Dr. Anthony Holmes, director of science and technology at the National Center for the Replacement, Refinement and Reduction of Animals in Research, created by the Government in 2004.
But do we even need real animals in the digital age?
Dr. Holmes says an international project is underway to develop a virtual dog (a computer model based on existing findings in dogs) that could be used to test the potential toxic effects of new drugs without using live animals.
Other projects include organoids, miniature versions of organs that can be grown in the lab for testing and research.
And there is artificial intelligence, where a computer could “learn” to predict what a drug might do.
But for now, animal research – despite its imperfections – is the best we have, says Dr. Holmes.
“I don’t think any scientist wants to work with animals, but until we have alternatives they will continue to be used.”