It was the gruesome fantasy spectacle that put mushrooms on the map.
The Last of Us, based on the popular video game of the same name, saw a group of intrepid explorers trudge across a dystopian American landscape in search of a way to defeat the uncontrollable fungus that co-opted billions of people’s brains and turned them into mindless, carnivorous zombies.
While the impact of fungal outbreaks in real life is not all that fantastic, there is more than a grain of truth in such a scenario, a leading expert in the field told DailyMail.com.
In fact, according to CDC fungal expert Dr. Ian Hennessee, the United States could soon be dealing with a rise in new fungal infections that can block breathing, cause nasty, agonizing boils to appear on the skin, or cause a fatal brain inflammation that ultimately results in death.
According to Dr. Hennesse, Blastomyces species is among the most pressing threats besides Candida auris and coccidioides, which cause valley fever, which is why he has dedicated most of his career to fungal research.
Dr. Hennessee said: “The Last of Us brought fungal diseases [to the fore]. They are often not the first ones the doctor will think of.
‘We are encouraging people to think about mushrooms because these mushrooms exist. They are often rare, but when people do have them, they are often misdiagnosed and underreported. And that can cause really serious illnesses.”
Dr. Ian Hennessee [pictured] is a disease researcher for the CDC specializing in fungal diseases. He helped lead a comprehensive surveillance project for a devastating blastomycosis outbreak at a Michigan factory last year.
Blastomycosis usually arises from exposure to humid environments, primarily in the upper Midwest. But epidemiological studies are increasingly finding the fungus on the East Coast.
Climate change is making the threat of widespread fungal diseases even more realistic, as warmer temperatures and wetter conditions allow species more time each season to thrive and spread their spores.
The fungus that causes valley fever, coccidioides, thrives in hot desert environments that are now increasingly hot and dry. And another, Histoplasma, which causes histoplasmosis, thrives in the moist soil of the East Coast, where it rains more and more each year.
In the West, Valley fever is making more people sick than ever, and cases in California tripled from 2014 to 2018 and from 2018 to 2022.
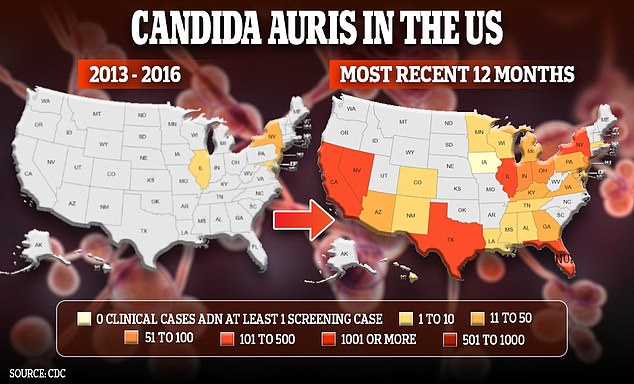
Meanwhile, Candida auris, a species of particular concern to disease researchers like Dr. Hennessee, infected about 2,400 Americans in 2022, up from 480 in 2019. Between 2013 and 2016, there were only 63 cases.
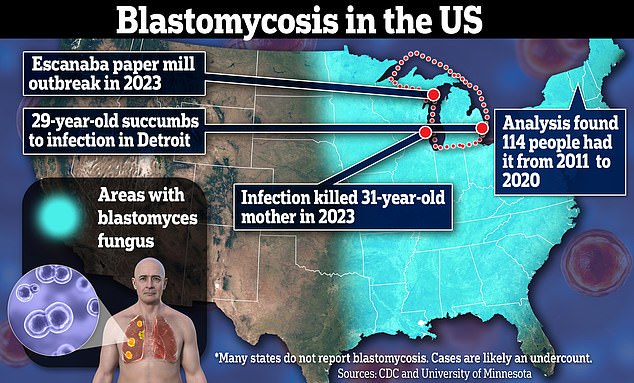
Blastomycosis, which results from breathing in spores of the fungus blastomyces, is also increasingly common. Last year, Dr. Hennessee helped investigate a massive outbreak at a Michigan paper mill that sickened more than 100 people and killed one.
And earlier this year, researchers found evidence of more than 100 cases of blastomycosis in Vermont, where the fungus blastomyces is not typically found.
Dr. Hennessee told DailyMail.com that climate change has helped the fungus expand its range, reaching new areas where it was not previously endemic, including Vermont. Developing drugs that can outlast the fungi’s ability to evade them is crucial to combating the public health threat.
He said: “As we see changes in environmental conditions, we are concerned about the change in the distribution, or even the impact of some of these fungal diseases, not just blastomycosis, but some others, histoplasmosis, valley fever and things So”.
In Michigan, Ian Pritchard, 29, became one of the first Americans in 2024 to succumb to blastomycosis, the second member of his family to die from it.
And in 2020, Ira Walker became infected. Ira languished in hospital for a month after doctors surgically cut an opening from his neck to his windpipe, before being transferred to a specialist facility to receive a higher level of care.

Ian Pritchard was in an induced coma in a Detroit hospital before dying from a fungal infection.
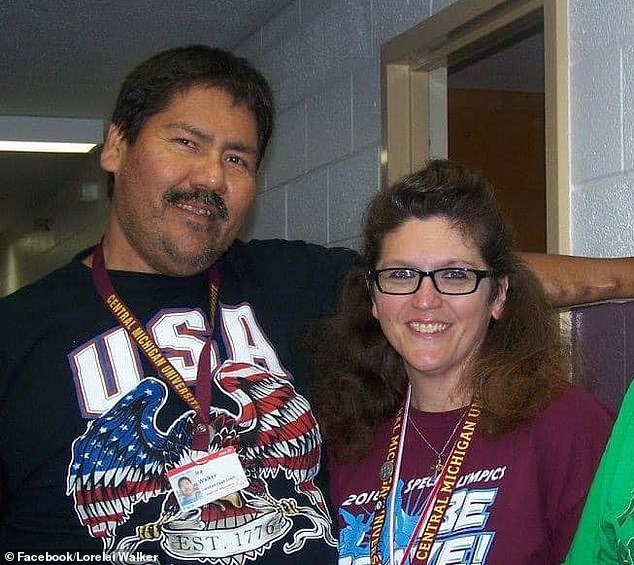
Ira Walker, pictured left, succumbed to blastomycosis in 2020. His wife Lorelei, right, told DailyMail.com she still doesn’t know how he got sick.
While the hope was that he would regain his lost strength and muscle mass, his situation only worsened.
His wife Lorelei told DailyMail.com: ‘Instead of regaining his strength, he became weaker. Every time the hospital called, there was news of another setback.
Blastomycosis is not reportable except in six states, meaning the federal government lacks a solid understanding of its exact prevalence.
When the spores are inhaled, the blastomyces fungus transforms into a type of yeast that embeds itself in lung tissue and appears as opaque masses on x-rays. For this reason, it is often confused with pneumonia.
People with the infection may suffer flu-like symptoms. In severe cases, they can progress within days or weeks to pneumonia, skin lesions (which appear as bumps, blisters, or ulcers), and neurological problems such as encephalitis or inflammation of the brain.
The infection is not transmitted from person to person. Instead, the fungus infects people when they breathe in its spores. It often hides in rotting wood and leaves.
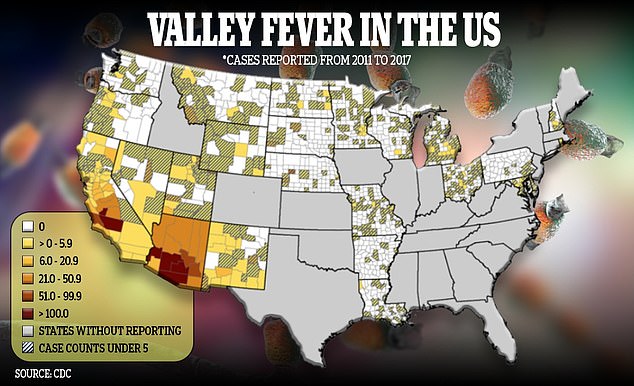
The fungus that causes Valley fever thrives in hot, dry environments
Although it can be found in the wood pulp that people handle in the early stages of paper production, the cases of blastomycosis at the Michigan paper mill were not limited to that part of the mill.
Dr. Hennessee said, “There was no smoking gun and no single place that we could point to and say, ‘Everyone got it here and no one got it there.'”
‘Instead, he pointed out to us something like: Well, could there have been some kind of broad environmental exposure? Maybe people are exposed as they, you know, park and walk to the mill, which is next to a river.
He added that the spores could have flown inside, possibly causing illness in the production stages.
Surveillance and warning efforts were extensive. Researchers like Dr. Hennessee ran around Escanaba, Michigan, knocking on doors and asking people if they worked at the plant, walked frequently, or rode ATVs through the woods.
He and his fellow researchers at the National Institute for Occupational Safety and Health held public meetings with employees.
Workers were eventually told to wear N95 respirators.
Deadly fungal diseases have become more common recently, from 4,746 cases in 2018 to 7,199 in 2021. And climate change appears to be driving this.
Dr Hennessee said: “We could see it in areas outside what we considered its historically endemic range.” We have never seen it before in a large industrial environment. [the Michigan outbreak] so we may sometimes see it in other areas where we just didn’t see it.”
He added: “But the evidence is limited. The evidence is limited.” We don’t have a lot of environmental sampling. And it’s not always easy to say, Hey, are you in a new place? Or is it just that we are looking for it in this new place?’
A 2022 report found that about 10 percent of blastomycosis cases are diagnosed in areas separate from where the fungus is known to thrive as warmer temperatures expand its endemic range.
A deadly combination of international travel and climate change is making infections more prevalent.
In Vermont, where winters are very cold and spring and summer are mild, it has become increasingly milder in the last decade, allowing non-native fungi to thrive.
Dr. Hennessee said: “We’re definitely concerned because temperatures are changing and environmental conditions are changing. And a lot of the fungi that we work with, including Blastomyces, are definitely very sensitive to climate or changes in temperature, precipitation and things like that. .
“The Vermont work is a good example, where we see it being detected in areas outside of what we thought was the historical range.”
Blastomycosis is much less common and not transmissible like another problematic disease-causing fungus, candida auris.
C. auris kills about one in three people who become infected. It is resistant to most antifungal infections, making it a cause of great concern to disease researchers.
The yeast is highly transmissible and spreads easily by touching contaminated surfaces among patients with weakened immune systems.
Infections can potentially trigger fatal sepsis. It is primarily a problem in healthcare settings and is rarely a problem for the general population.
Dr Hennessee said: “It can cause more types of healthcare-related outbreaks and can spread quite quickly.” And it is often very resistant to medications as well.
“We worry about it, and it’s spreading pretty quickly globally, specifically in healthcare settings.”


![EXCL: CDC’s Fungal Fighter Reveals Why the Next Pandemic Could Dr. Ian Hennessee [pictured] is a disease researcher for the CDC specializing in fungal diseases. He helped lead a comprehensive surveillance project for a devastating blastomycosis outbreak at a Michigan factory last year.](https://whatsnew2day.com/wp-content/uploads/2024/04/EXCL-CDCs-Fungal-Fighter-Reveals-Why-the-Next-Pandemic-Could.jpg)