Doctors and scientists have put forward controversial proposals that will allow healthy middle-aged adults to be diagnosed with Alzheimer’s disease, even if they have no symptoms and may never develop the disease.
The plans, which come from an influential US-based Alzheimer’s Association panel, involve radically expanding the definition of the disease to include millions of people who do not have cognitive or memory problems.
But people with abnormal levels of a toxic protein called amyloid, which builds up in the brain and has been linked to the development of Alzheimer’s, could be told they are in a new “stage one” of the disease, despite to be apparently healthy.
The plans, discussed at an international dementia conference, have been driven in part by the availability of new blood tests that can easily detect high levels of amyloid long before symptoms appear.
Scientists backing the move also point to innovative new drugs such as lecanumab and donanemab (already approved in the US and soon to be given the green light in the UK) that have been shown to clear the brain of amyloid and have a small effect on slow down the condition.
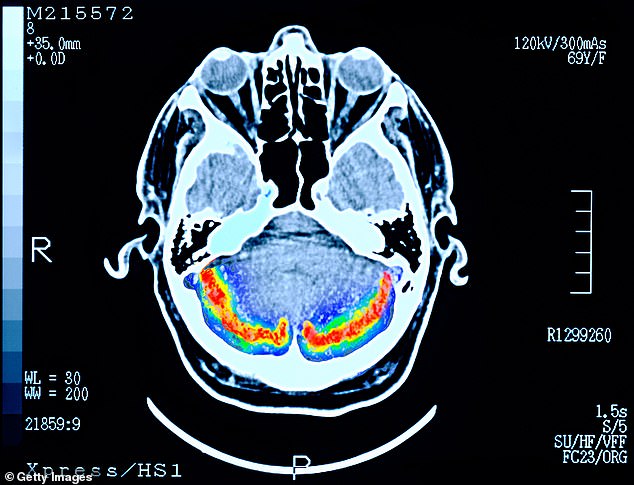
LIFE ALTERING: A brain scan of a patient with early stage dementia
In trials, the modest benefits of these treatments were seen only in those with very early-stage Alzheimer’s. Scientists say that if given before symptoms begin, they may be more effective.
One of the panel members, María Carrillo, chief scientific officer of the Alzheimer’s Association, said: “The purpose of this initiative is to advance the science of early detection and treatment. To prevent dementia, we must detect and treat the disease before symptoms appear.’
But the proposals have sparked a backlash, as leading doctors warn of the “very serious” dangers of diagnosing healthy adults with a life-altering disease that they may never develop.
Robert Howard, professor of aging psychiatry at the UCL Institute of Mental Health, says there is still much more to understand about the specific role amyloid plays in the development of Alzheimer’s. He points to research that suggests that many older people have a substantial buildup of amyloid in the brain but never show any outward signs of the disease.
“The majority of people without evidence of cognitive impairment who test positive for amyloid will never develop dementia,” says Professor Howard. ‘If you tell them they have Alzheimer’s, they will worry for the rest of their lives. Some will make decisions about their lives based on a false premise. And evidence shows that some may become depressed or even suicidal.’
Dementia kills 60,000 people in the UK each year and Alzheimer’s is the most common type. It’s still unclear what causes it, although the leading theory is that toxic proteins called amyloid and tau accumulate and clump in the brain, forming plaques and causing inflammation. Whether the plaques cause the disease or are a symptom of it, or both, remains debated.
Despite this, the panel has suggested revising the diagnosis of Alzheimer’s to include six stages of the disease, depending on the existence of plaques and symptoms.
Stage one involves those who have no symptoms but have high levels of amyloid. They would move to Stage Two if they developed neurological problems such as anxiety or depression, even though these are not necessarily related to dementia.
The third stage is for those with mild cognitive impairment: those with thinking and memory problems but who can normally continue with their daily lives.
Stages four, five and six of the disease are associated with mild, moderate or severe dementia.
“There are already doctors in the US who are thinking about Alzheimer’s in this way and offering patients these blood tests in their clinics,” says Professor Howard, “but I don’t know any sensible doctors in the United Kingdom that thinks it is a good option. idea. For one thing, treatments are extremely limited, even if you have symptoms.
“At the moment, these blood tests should only be available to patients with diagnosed dementia, who have symptoms and want to know what type of dementia they have.”
Doctors at UK memory clinics use amyloid blood tests as an alternative to expensive PET scans and invasive lumbar punctures to help differentiate between someone with vascular dementia, Alzheimer’s disease or other forms of the disease.
All Alzheimer’s patients will have abnormal levels of toxic proteins, but there is currently no way to know which patients with abnormal blood test results and no symptoms may or may not end up with Alzheimer’s.
Lecanumab and donanemab have been shown to clear the brain of toxic plaques in people with Alzheimer’s disease who already have symptoms, but they have also been linked to serious complications, such as brain hemorrhages and swelling.
“There is an argument that the reason they haven’t worked very well so far is that they weren’t given early enough,” says Professor Howard.
‘Could they work better if given before symptoms start? It’s an interesting question, and part of this push to diagnose early is because drug companies, some scientists and charities are so motivated to try it.
‘Some asymptomatic people who tested positive for amyloid blood tests in the US are already being recruited for new trials. But thousands of people would have to be treated for up to 20 years to show if it can really make a difference.’
Other members of the Alzheimer’s Association panel include scientists who work with companies that are developing anti-amyloid drugs. The charity has denied that these links affected its proposals.
However, his skeptics have stopped short of saying that an approach like this could never work.
“If one day we had an effective treatment that could be taken long before symptoms started and prevent dementia, that would be fantastic,” says Professor Howard.
“But there is no indication or suggestion that anything like this is on the way any time soon.”
WHAT IS THE DIFFERENCE… between tonsillitis and strep throat?
Tonsillitis is an infection of the tonsils in the throat. It is more common in children and the main symptoms are sore throat, problems swallowing and high temperature.
Doctors do not usually offer treatment for tonsillitis, as it usually goes away on its own.
Strep throat is an infection of the back of the throat (and sometimes the tonsils) caused by a bacteria called streptococcus A. It is also most commonly found in children, and although the symptoms are similar to tonsillitis, it can cause red rashes, white pus in the throat, and difficulty breathing.
Most strep infections can be treated with antibiotics, but they can sometimes lead to a life-threatening condition called invasive group A strep.
THIS WORKS
Enterosgel Children


A gel that is mixed with water to help combat upset stomach and diarrhea. This new unflavored version is designed specifically for children.
90g for £12.95, enteromed.es
