The Biden administration unveiled its latest effort to cancel millions in student loan debt that the White House said would provide relief to up to 30 million borrowers.
The effort comes after the Supreme Court last year blocked President Biden’s first plan for widespread student loan debt forgiveness.
After the original plan was rescinded, the Biden administration began looking for other ways to cancel the debt through the rulemaking process. Monday’s new proposals are the result of those efforts.
The new plans would cancel up to $20,000 in unpaid interest for borrowers who currently owe more on their loans than they originally borrowed.
The cancellation of interest would affect single borrowers earning $120,000 or less and married borrowers earning $240,000 or less and would be carried out automatically without borrowers having to apply.
The plans would also cancel the debt of two million borrowers who would have qualified for other forgiveness programs but have not yet applied.
Additionally, college borrowers who began repayment 20 or more years ago, graduate student borrowers who began repayment 25 or more years ago, borrowers who have been enrolled in programs of low financial value, and those who have faced financial hardship Pay off your loans also see relief.
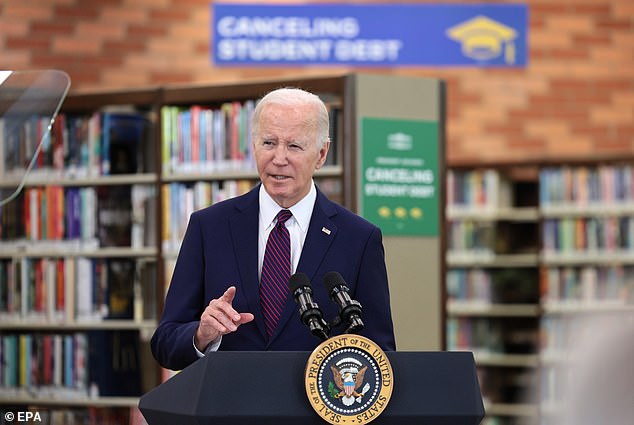
Biden spoke in California in February after the White House announced the cancellation of $1.2 billion in student loan debt under the SAVE plan.
According to the Biden administration, the plans would completely eliminate accrued interest for 23 million borrowers, cancel the entire amount of student loan debt for more than four million borrowers, and provide more than 10 million borrowers with at least $5,000 or more in debt relief.
The administration will unveil plans in the coming months, which will then face a public comment period. Senior administration officials said the goal is to begin providing aid this fall.
“President Biden will use every tool available to cancel student loan debt for as many borrowers as possible, no matter how many times Republican elected officials try to stand in his way,” said White House Press Secretary Karine Jean -Pierre, in a call to journalists.
Administration officials will fan out across the country on Monday to promote the latest efforts. President Biden will outline the new plans Monday during a visit to Madison, Wisconsin.
Secretary of Education Miguel Cardona will also promote the new proposals during a visit to New York, Vice President Harris will travel to Philadelphia, and Second Gentleman Doug Emhoff will highlight the effort in Phoenix, AZ.


The Biden administration has canceled nearly $144 billion in student loan debt despite the Supreme Court blocking the president’s first student loan forgiveness plan.
Last June, the Supreme Court blocked the president’s original $400 billion plan to cancel up to $20,000 in student loan debt for millions of borrowers earning less than $125,000 a year.
But the Biden administration said it was not over its fight to provide relief to millions of borrowers.
Senior administration officials said they carefully studied the Supreme Court’s 2023 decision and applied the new regulations in a manner consistent with that decision.
The new plans are part of the regulatory process that began last summer and are being carried out under the authority of the Secretary of Education in the Higher Education Act.
“This is not the same plan and we feel confident moving forward,” a senior administration official said.
Monday’s announcement of additional student loan debt cancellation adds to other efforts the Biden administration has already made since the first plan was blocked.
To date, the Biden administration has already canceled $146 billion in student loan debt for four million borrowers through changes to multiple programs, including the income-driven repayment plan and fixing the Public Service Loan Forgiveness program. .
Just months after the highest court blocked Biden’s first student debt plan, the administration also launched the Saving on a Valuable Education, or SAVE, plan.
The SAVE plan is an income-generating repayment plan that reduces the amount of time and money some borrowers have to repay before their student loan debt is forgiven.
In February, the administration began paying off billions of debt under the SAVE plan, including $1.2 billion for 153,000 borrowers.
The White House said more than 7.7 million borrowers have enrolled in the plan and was encouraging millions more to do so.
The Department of Education said it would continue to identify borrowers who qualify to have their debt forgiven on an ongoing basis.
Critics of the White House’s efforts argue that canceling student loan debt is unfair and a burden on taxpayers who chose not to pursue an expensive college education or take out massive student loans.
Republicans have also accused the White House of trying to curry favor with young voters before the November election by canceling their student loan debt.
As the Biden administration launches its latest student loan forgiveness effort, the SAVE program already faces a legal challenge.
On March 28, 11 states led by Kansas filed a federal lawsuit in an effort to block the forgiveness program. The lawsuit argued that the effort is no different than the president’s first attempt to eliminate student loan debt that was rejected by the Supreme Court.
Republican Kansas Attorney General Kris Kobach has vowed to take the case all the way to the Supreme Court if necessary.
Along with Kansas, the lawsuit is backed by Alabama, Alaska, Idaho, Iowa, Louisiana, Montana, Nebraska, South Carolina, Texas and Utah.
Last June, the Supreme Court ruled that the Biden administration had overstepped its authority with its original plan that relied on the HEROES Act, a law that authorizes the Secretary of Education to forgive or modify federal student loans due to an emergency. national.
The same day he was blocked, Biden said the administration would seek debt forgiveness through a different legal authority in the Higher Education Act of 1965.
Senior administration officials said they are not concerned that the move to cancel millions in student loan debt will have an inflationary effect based on analysis by the Council of Economic Advisers.
They argued that the measure would have a positive effect on economic growth and the economic mobility of American families.
More than 43 million Americans have more than $1.6 trillion in federal student loan debt.
