A worrying development in the H5N1 avian flu outbreak occurred in Missouri last week.
For the first time, the virus was diagnosed in a patient who had not been in contact with sick birds, cows or other animals.
The worst-case scenario is that the patient contracted the virus from someone else and the virus began to spread silently among Americans.
While this is unlikely, Dr. Kruitka Kuppali, a spokesperson for the Infectious Diseases Society of America and a former World Health Organization official, warned this week: “This is how pandemics start.”
Experts told DailyMail.com the situation is “somewhat similar” to how previous pandemics began, although they insisted there is “no need to panic” just yet.
Experts told DailyMail.com that while it is highly unlikely, bird flu looks “somewhat similar” to the early days of the Covid pandemic (stock)
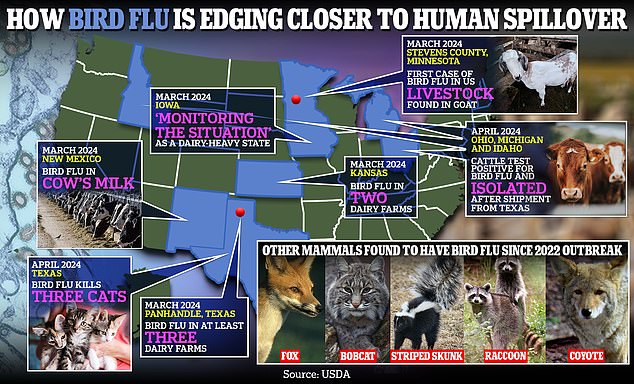
The above shows how bird flu is moving closer to human spread in the US.
For example, the 2009 swine flu pandemic was first detected in a similar way: when two children in California were diagnosed with the flu who had had no contact with pigs or each other.
The initial Covid outbreak in China also began with cases of a mysterious flu-like illness, and no apparent connection emerged in Wuhan.
Missouri health officials have declined to say how the state’s “patient zero” became infected, only that the risk to the public remains “low.”
Still, experts are concerned about the case and the lack of transparency.
Dr Raj Dasgupta, chief medical adviser at Fortune Recommends Health, told DailyMail.com: ‘When health authorities are not transparent, it can cause problems.
‘If people don’t receive clear information, they may not know what symptoms to look for, what actions to avoid, or how to protect themselves.
‘This can cause confusion, spread false information and create unnecessary fear, making it difficult to confront a potential health threat.
‘Health officials need to share clear and accurate information quickly to prevent outbreaks and maintain public trust.’
The Missouri case was detected through the state’s seasonal flu surveillance system, which tracks influenza activity based on testing of symptomatic patients.
Because bird flu doesn’t always cause symptoms, there could be more people who are sick who were never tested.
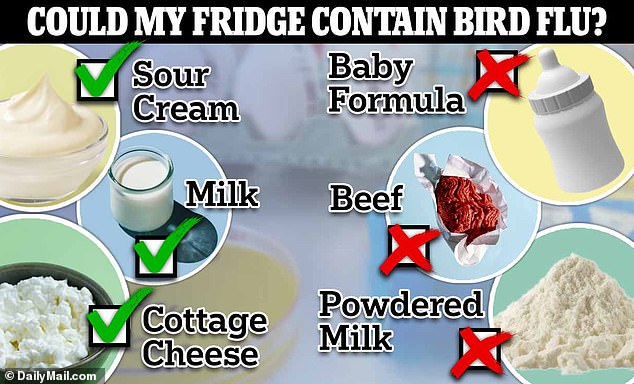
A check mark indicates foods that tested positive for bird flu, while a cross indicates those that were tested for bird flu but were not found to contain the virus.
Another theory is that the patient drank raw milk that was contaminated with the virus.
Raw milk is becoming increasingly popular and studies have shown that H5N1 particles can remain in it for up to five weeks if refrigerated, according to the National Institutes of Health (NIH).
About four percent of Americans (nearly 11 million) consume raw milk and raw cheese, which do not undergo pasteurization, a process that uses heat to kill about 99.9 percent of pathogens.
In April, the WHO warned that bird flu had been detected in “very high concentrations” in samples of raw milk, but that pasteurized milk, commonly sold in major retailers, was safe to consume.
In recent years, fitness enthusiasts and wellness influencers have hailed raw milk as a superfood, claiming that it contains more vitamins and minerals than pasteurized milk and is better tolerated by people with asthma and lactose intolerance.
However, the CDC classifies raw milk as “one of the riskiest foods” and says the germs it can carry “can pose serious health risks to you and your family.”
Dr Thomas Peacock, an influenza virologist at the Pirbright Institute in the UK, said: Statistics NewsThe obvious question I’d like to ask is: Have you ruled out someone who has a large container of raw milk in the refrigerator? Because that seems like an obvious route for a cryptic infection.
Lisa Cox, a spokeswoman for the Missouri Department of Health, said the patient had not reported consuming raw milk.
However, it is unclear whether officials actually investigated this or simply asked the patient directly.
Dr. Peacock also warned that the patient may have had an outdoor cat, as several free-range cats have died from the virus this year. He noted that if the patient had a cat, it could have drunk raw milk from a
Raw milk is not prohibited in Missouri, although it can only be legally purchased directly from a farm or from farmers market vendors with a permit.
Raw milk is not the only food that carries risk.
Dr Darin Detwiler, a food safety expert at Northeastern University in Boston and a former adviser to the FDA and USDA, previously told DailyMail.com that foods with undercooked meat or eggs could also harbour small fragments of bird flu and other deadly diseases.
He noted that while the risk is “very low,” cooking these foods thoroughly is essential to kill all pathogens. For example, searing a steak on the outside “should be enough to kill a pathogen, even if the inside is not cooked thoroughly,” since bird flu could move into the inner part of the meat.
Dr. Detwiler also recommends clients be wary of eggs that have runny yolks, which includes fried, poached, soft-boiled and deep-fried eggs.
“If there is concern about bird flu, eggs should be cooked until both the white and yolk are firm, ensuring the egg reaches a temperature likely to kill any virus present,” he said.
According to the USDA, eggs should be cooked to at least 160 degrees Fahrenheit (71 degrees Celsius).
Dr. Eve Elizabeth Pennie, General Practitioner and Medical Fellow at Drug surveillancetold DailyMail.com that “while transmission of bird flu through food is not standard, following safe food practices is always the best way to protect yourself and your family.”
Dr Dasgupta also noted that while human-to-human transmission is highly unlikely, spreading bird flu in this way could pose serious outbreak risks.
“If the virus is spreading between people, it could mean it has changed or adapted to spread more easily, which could lead to larger outbreaks or even a pandemic,” he said.


