Stress and anxiety may partly explain why colon cancers are increasing among younger generations of Americans, a study suggests.
Researchers from China’s Sichuan University found that under frequent stress, a number of healthy bacteria living in the intestine begin to die, making it easier for cancer to enter.
They found that when these bacteria die, the tumors grow more rapidly, leading to more aggressive and fast-growing colorectal cancers.
These findings come amid a rise in colon and rectal cancers in young people in the US and UK, which experts had previously attributed to diet.
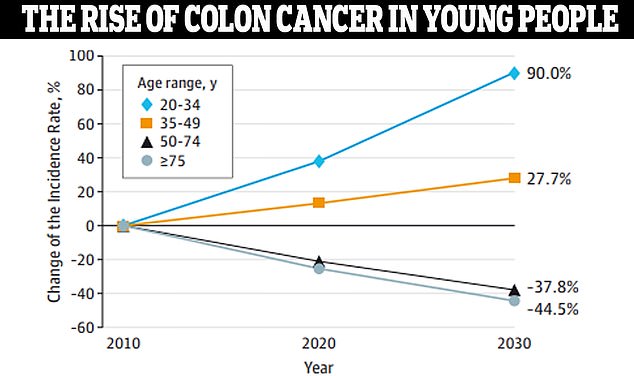
Data from JAMA Surgery showed that colon cancer is expected to increase by 90 percent in people ages 20 to 34 by 2030.
However, an emerging area of science suggests that the gut and the body’s microbiome may play a role.
At the same time, data shows that more young Americans and Britons than ever are constantly stressed, anxious or depressed. Surveys have consistently shown that younger generations are more stressed than any other demographic group.
A 2023 survey of the American Psychological Association found that the average person between the ages of 18 and 34 rates their stress level as a six out of ten, while people ages 65 and older rate their stress level slightly above a three.
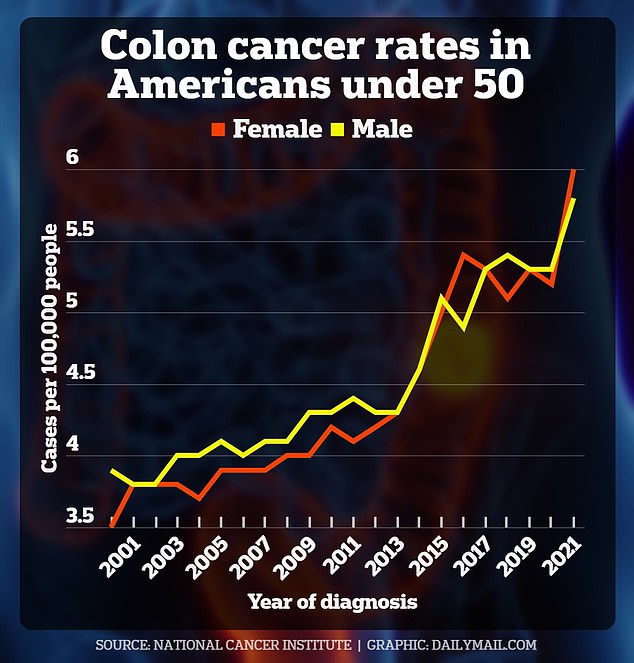
The United States has the sixth highest rate of early-onset cancers (87 cases per 100,000 people) and colorectal cancers (CRC) are among the fastest growing.
Diagnoses among people under age 50, who are classified as early-onset, are expected to increase by 90 percent in people ages 20 to 34 between 2010 and 2030.
Several factors are suspected of causing the increase in the disease in young people: a diet of highly processed foods and energy drinks, obesity, a disruption of beneficial bacteria in the intestine and, more recently, high blood sugar. the blood
Overuse of antibiotics has also been postulated as a factor, but a separate study study in the journal Clinical Gastroenterology and Hepatology, found that research examining this link reported conflicting findings and the most recent results were not statistically significant.
When taken in moderation, antibiotics are very effective and safe treatments for bacterial diseases and these medications have revolutionized the way doctors fight infections.
But when taken too frequently, they can cause a major disruption to the healthy colonies of bacteria that live in the gut—the body’s microbiome.
Therefore, the Chinese team used a cocktail of antibiotics to test their theory.
The research was presented at the United European Gastroenterology Week 2024, but has not yet been published in a journal or peer-reviewed, meaning that all the details of the study, carried out on mice, are unknown.
Lead researcher Dr Qing Li said: “In our study, we used an antibiotic cocktail to eradicate the gut microbiota, followed by fecal microbiota transplantation to investigate whether gut microbiota was necessary for chronic stress to accelerate progression of CRC”.
Fecal microbiota transplant is a scientific term that means researchers transferred healthy feces into the body of someone with a diseased gut, with the goal of repopulating their gastrointestinal tract with healthy bacteria.
They supplemented mice that had CRC with a healthy poop sample, exposed them to stress, and watched what happened to the cancer’s progression.

The bacteria Lactobacillus plantarum lives naturally in the intestine and in some fermented foods. Researchers found that when they were absent from intestinal cells, tumors grew more easily
In another group of mice with CRC, they introduced antibiotics to kill bacteria in the intestine and exposed the animals to stress.
In mice without gut bacteria, tumors grew faster than when they had a robust microbiome to protect them.
Furthermore, even when no antibiotics were introduced into the system, researchers showed that stress alone can weaken the microbiome, making the body more susceptible to tumors.
Therefore, stress alone could increase the likelihood of colorectal cancer and tumors, the study authors suggest.
One group of bacteria in particular seemed to be especially affected by antibiotics and stress: lactobacillus.
Older research Trinity College in Ireland It has been suggested that these bacteria support the body’s immune system, may protect against viruses and bacteria, and prevent damage to intestinal cells.
This bacteria is found naturally in many fermented foods and in the human body. When the body was exposed to antibiotics, the lactobacillus was completely depleted in both groups tested.
Dr Li said: “This depletion highlights its crucial role in maintaining intestinal health and its possible association with CRC progression under chronic stress.”
“Restoring beneficial bacteria in the gut, such as Lactobacillus, could strengthen the body’s natural defenses against colorectal cancer.”
Doctors could harness Lactobacillus in the future to treat CRC cancer, Dr. Li suggested.
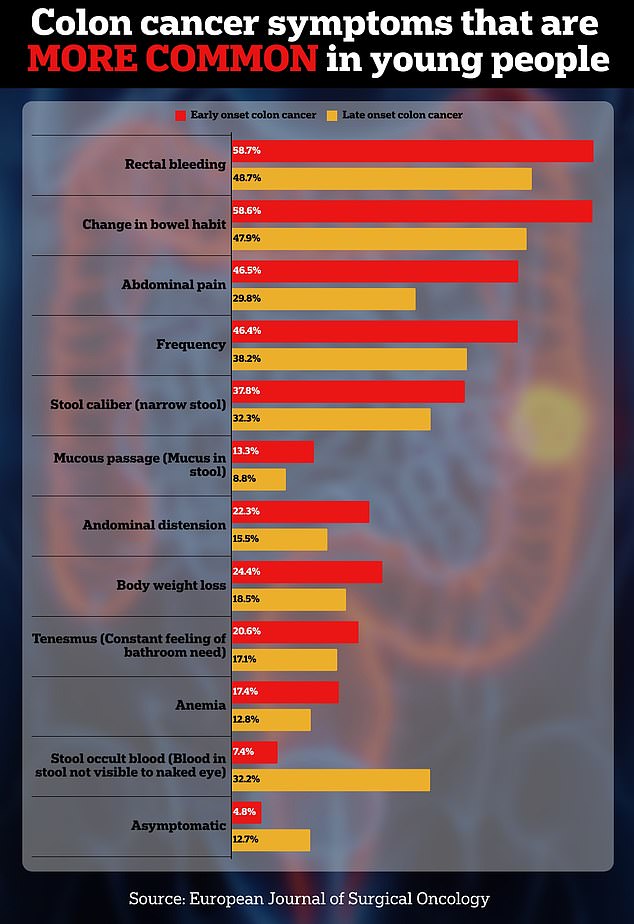
The above shows the symptoms and their frequency in early-onset patients, who develop colon cancer before the age of 50, and late-onset patients, who develop cancer after this age.
There are an estimated 100 trillion bacteria living in and around the digestive tract (more than the number of cells in the body), according to research by Emory University.
They help keep the area lubricated, help the body break down food, and can even make neurotransmitters and vitamins that the body needs to function.
Research from the University of Missouri-Kansas City found that the rate of colorectal cancer increased 500 percent among children ages 10 to 14 and 333 percent among adolescents ages 15 to 19.
Rates rose 71 percent among people ages 30 to 34, to seven cases per 100,000 people. And among people ages 35 to 39, rates rose 58 percent to 12 cases per 100,000 people.
Rates of colorectal cancer in people ages 10 to 44 have increased in all age groups.
The rate of colorectal cancer increased by 500 percent among children ages 10 to 14 and 333 percent among adolescents ages 15 to 19.
Rates rose 71 percent among people ages 30 to 34, to seven cases per 100,000 people. And among people ages 35 to 39, rates rose 58 percent to 12 cases per 100,000 people.