They have been blamed for a range of symptoms, from insomnia to sexual problems.
But a major new study appears to provide evidence of another side effect: weight gain.
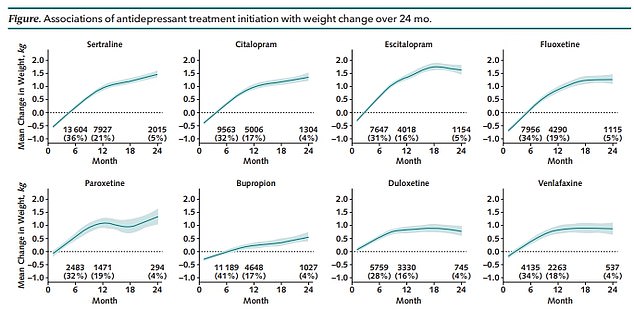
Harvard researchers studied prescription data from nearly 200,000 American adults and found that those who took escitalopram, paroxetine and duloxetine tablets gained up to three pounds after two years of taking the drugs.
Those taking those drugs were 10 to 15 percent more likely to gain at least five percent of their initial weight, compared with users of five other commonly prescribed antidepressants, such as sertraline.
In comparison, other drugs such as duloxetine or Cymbalta were associated with only one pound of weight gain over a two-year period.
The graph above shows the difference in average weight gain between the eight antidepressants studied.

The unpleasant side effect may be enough to convince people to stop taking a drug that could save their lives.
All eight drugs studied were associated with some weight gain over a two-year period.
However, the smallest weight gain was seen in patients who took bupropion or Wellbutrin (one of the three drugs studied that is not an SSRI) and who gained less than a pound around their waist.
Only duloxetine and paroxetine were associated with no weight gain after six months.
Researchers studied weight changes at 6, 12, and 24 months after starting one of eight common antidepressants: sertraline, citalopram, escitalopram, fluoxetine, paroxetine, bupropion, duloxetine, and venlafaxine.
All participants were not required to have taken antidepressants in the six months prior to the study, although it was not possible to confirm whether such medications had been prescribed before that period.
While anecdotal reports of weight gain are common, the FDA does not mention it as an official side effect of most SSRIs.
One in ten Americans takes antidepressants, which are a highly effective tool to help dispel the fog of depression and anxiety disorders.
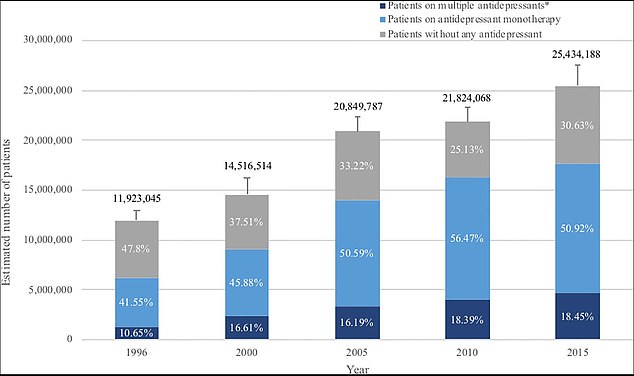
The graph above shows antidepressant treatment for patients with major depression over the past 20 years.
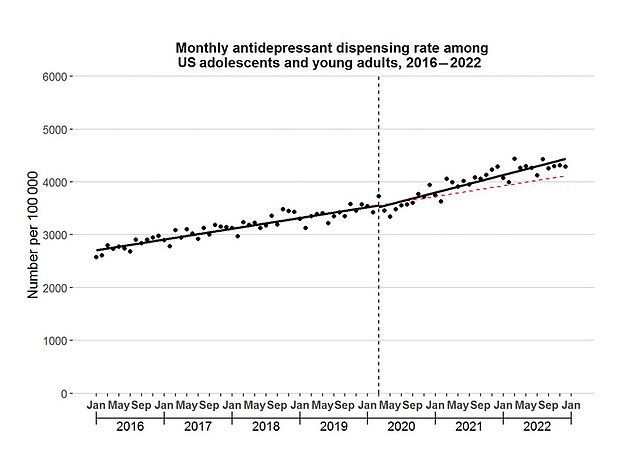
Monthly antidepressant dispensing rate among US adolescents and young adults aged 12–25 years, 2016–2022. Vertical line represents March 2020, the beginning of the US Covid outbreak.
A study earlier this year found that antidepressant prescriptions for young adults and teens have increased nearly 64 percent since 2020.
Dr Joshua Petimar, a professor in the Department of Population Medicine at Harvard’s Pilgrim Health Institute and co-author of the new study, said of their findings: “Patients and their doctors often have several options when they first start taking an antidepressant. This study provides important real-world evidence about how much weight gain to expect after starting some of the most common antidepressants.
‘Doctors and patients can use this information, among other factors, to help decide which option is best for them.’
The study, published in the Annals of Internal Medicine, did not include a control group (in which weight gain was compared to that of someone not taking the drug).
This means that the small weight gain over a two-year period could be due to chance or to the mental health problem itself.
Dr. Petimar and other researchers at Harvard Medical School and the Harvard Pilgrim Health Care Institute analyzed prescription data from eight U.S. health systems that are part of PCORnet, the National Patient-Centered Clinical Research Network.
They studied 183,118 adults between the ages of 18 and 80 who had recently started taking one of eight common antidepressants.

Bupropion, marketed as Welbutrin, was the least likely to cause patients to gain extra pounds up to two years after starting the regimen.

The risk of gaining at least 5% of initial weight was 15% lower with bupropion (Welbutrin) and higher with escitalopram (Lexapro).
After six months of use, patients taking escitalopram, paroxetine, and duloxetine gained approximately 0.66 to 0.88 pounds more than patients taking sertraline, and were 10 to 15 percent more likely to gain at least 5 percent of their initial weight.
Dr Jason Block, lead author, a general internal physician and professor at Harvard Medical School, said: ‘While there are a number of reasons why patients and their doctors might choose one antidepressant over another, weight gain is a major side effect that often leads patients to stop their medication.
“Our study found that some antidepressants, such as bupropion, are associated with less weight gain than others. Patients and their physicians may consider weight gain as a reason to choose the medication that best suits their needs.”
Some antidepressants are thought to increase appetite, leading a person to consume more calories.
Selective serotonin reuptake inhibitors are the most commonly prescribed type of antidepressant.
Common SSRIs include fluoxetine, citalopram, sertraline, paroxetine, and escitalopram.
Doctors also often prescribe serotonin and norepinephrine reuptake inhibitors (SNRIs). The most common SNRIs are venlafaxine and duloxetine.
Bupropion, or Wellbutrin, is a dopamine/norepinephrine reuptake inhibitor (NDRI).
It is not fully understood how these medications work to control anxiety and improve mood, but experts believe it is due to the impact the drugs have on crucial hormones in the brain.
SSRIs specifically increase serotonin levels in the brain by inhibiting the reuptake (absorption) of serotonin into brain cells.
This makes more serotonin available to improve the transmission of messages between neurons.
Serotonin and norepinephrine reuptake inhibitors, on the other hand, increase the levels of serotonin and norepinephrine in the brain. They inhibit the reuptake of these two neurotransmitters, making them more available to improve communication between neurons.
By increasing the levels of these neurotransmitters, it is said to reduce anxiety, improve mood, and increase overall emotional well-being.
Other recognized side effects of antidepressants include nausea, dizziness, restlessness, and sexual dysfunction.
Some patients report that sexual problems continued for years after stopping SSRIs, but large, high-quality studies have not yet demonstrated this conclusively.
Psychiatrists say antidepressants are highly effective at treating mood disorders, and some studies suggest the pills saved at least 30,000 Americans from suicide between 1988 and 2002 alone.