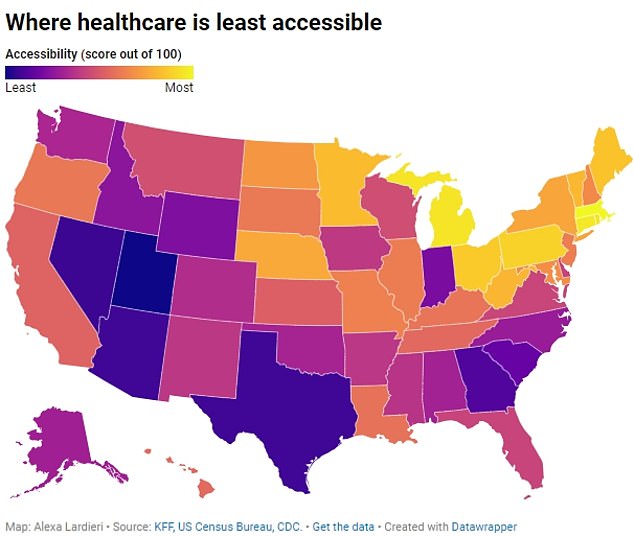
Americans in the western part of the country are struggling to receive adequate and timely health care.
Utah, Nevada and Arizona are among the worst for access to health care, struggling with a lack of resources, too few qualified doctors and having large swaths of uninsured residents.
Meanwhile, Americans in the New England area enjoy much more affordable health care, with Massachusetts, Connecticut and Rhode Island among the best states for access to health care.
These states have more hospital beds and primary care doctors, as well as fewer uninsured residents.
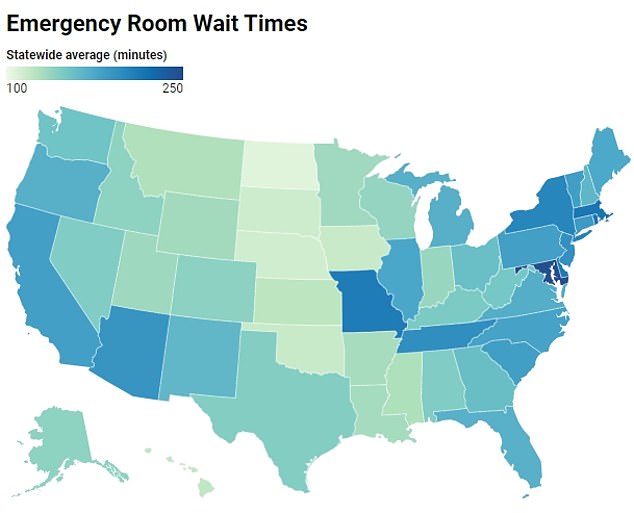
However, patients in these states still face long wait times for emergency department visits and doctor appointments due to their dense populations.
A Forbes analysis found that Utah is the least accessible when it comes to health care services.
The analysis, carried out by Forbes and based on KFF data, Centers for Disease Control and Prevention and the US Census Bureau.measured 14 metrics.
These included the number of doctors, nurse practitioners and physician assistants in the state, the percentage of uninsured residents, the number of hospital beds and how many people have delayed care because of costs.
States were then rated on a scale from zero to 100, with zero indicating that the state had the most accessibility to health care and 100 indicating that the state had the least accessibility to health care.
Utah topped the list with a score of 100 due to its lack of resources, including fewer qualified professionals.
Additionally, Utah employers cover the second-lowest percentage of employees’ annual health costs and eight percent of residents are insured.
As a result, 11 percent have delayed visiting the doctor due to high costs.
Utah also has the third-lowest number of primary care physicians per 10,000 residents (11.3) and the fewest hospital beds per 1,000 residents (1.7).
It ranked fourth-lowest in number of nurse practitioners (3.9 per 10,000 people) and the state has the eighth-lowest number of physician assistants: two per 10,000 people.
Nevada follows with a score of 93 out of 100. Its high inaccessibility score is because the state has the fewest primary care physicians in the country (10 per 10,000 residents) and the second-lowest number of practical nurses. advanced (one per 10,000). people.
Additionally, 11 percent of its residents are uninsured, ranking sixth in the country, and 13 percent have delayed medical care due to costs.
With a score of 92.15, Texas rounded out the three least accessible states.
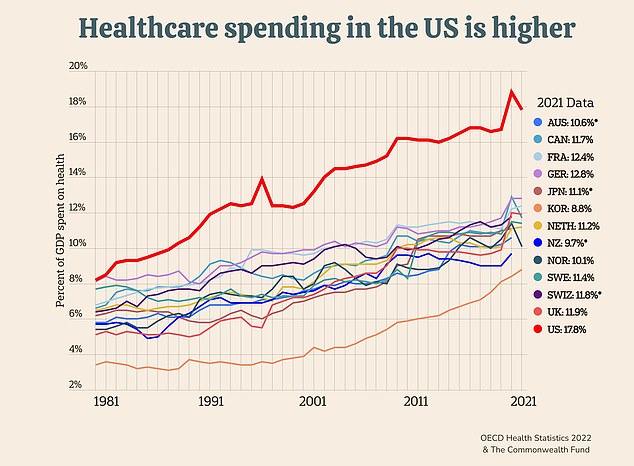
Total U.S. health care spending, which includes what the government, insurance companies and individuals pay, surpassed $4.3 trillion in 2021, nearly a fifth of the country’s annual GDP.
The Lone Star State has the highest percentage of uninsured people (nearly 17 percent) and the highest percentage of residents (16 percent) who delayed a doctor’s visit because of cost.
This delay or lack of care could be why Texas has 300 more preventable hospital admissions per 100,000 patients than the national average of 2,765, aAccording to US News Best States classifications.
To make matters worse, a report of the Center for Healthcare Quality and Payment Reform (CHQPR), found that nearly half of the state’s rural hospitals (75) are at risk of closure.
Among the 50 states, this is the largest number of rural hospitals at risk and could lead to worse healthcare accessibility.
While Western Americans may struggle with health care, people in the northeastern U.S. enjoy abundant and more affordable health care.
Massachusetts, Connecticut, and Rhode Island are the three states with the highest accessibility to health care.
Massachusetts, home to some of the top-ranked hospitals, scored a zero in Forbes’ analysis.
Only two percent of residents are uninsured (the lowest in the country) and the state has the highest ratio of primary care physicians to residents and specialists to residents at 23 per 10,000 and 30 per 10,000, respectively.
It also has the fourth-lowest percentage of people delaying care because of costs.
Additionally, its top-notch health care system could be a factor behind the state’s lowest infant mortality rate nationally, second-lowest obesity rate and third-lowest smoking rate in the state, according to a report. separate from US News. analysis.
Connecticut ranked second with an accessibility score of 4.2 out of 100. The state is home to the highest number of physician assistants per 10,000 residents (7.3) and has the third lowest smoking rate.
Rhode Island rounded out the top three with a score of 4.5. It has the fourth-lowest percentage of uninsured people (4.2 percent) and the lowest percentage of residents delaying medical care (7.7 percent).
It also ranks fifth in infant mortality and sixth in overall mortality rate.
The national discrepancy could be due to geographic differences between states, as the most accessible states have major cities where densely populated residents can easily access the best hospitals and medical research facilities.
While less accessible states tend to have more rural cities and the population tends to be more dispersed, meaning people are further away from hospitals, clinics and doctors’ offices.
In Utah, 12 percent of the population lives in nonmetropolitan areas, compared to just 1.5 percent in Massachusetts.
However, being in a big city can also have its disadvantages. While care may be accessible, more people fight for it.
In a separate analysis conducted earlier this year, Massachusetts was found to have the second-longest wait time in the emergency department, at 214 minutes.
Connecticut was 10th with 186 minutes and Rhode Island was third, with a wait time of 214 minutes.
Furthermore, a 2023 analysis found that the average wait time for a doctor’s appointment in Boston, Massachusetts, was 34 days, above the average in 15 major cities, which was 26 days.
The AMN Healthcare and Merritt Hawkins analysis attributed the long wait times to a growing population, an increasingly elderly population requiring more care and doctors leaving the field due to burnout.
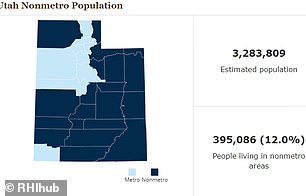
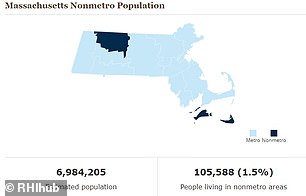
In Utah, 12 percent of the population lives in nonmetropolitan areas, compared to just 1.5 percent in Massachusetts.
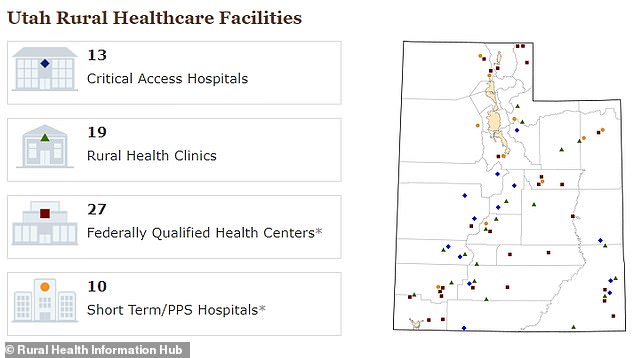
In Utah, rural hospitals are spread throughout the state and some areas do not have health clinics.
While some U.S. states fare better than others, overall, the quality and accessibility of health care in the U.S. is inferior compared to comparable countries.
The United States spends about twice what its peer countries spend on health care for its residents; However, Americans live shorter lives and are more likely to suffer from chronic illnesses or die by suicide.
Compared with other wealthy nations such as Japan, Switzerland, France and Australia, Americans die on average three years earlier, more likely that their deaths would have been prevented with better access to care.
The United States also has the highest maternal mortality rates: 24 new mothers die for every 100,000 babies born, almost two and a half times the average of other wealthy countries and 19 times higher than the best-performing country on the list, the Netherlands. .