Experts have warned that prostate cancer screening may be doing more harm than good, as a shocking study showed one in six cases flagged during a 15-year trial was wrong.
This is the largest investigation into the prostate-specific antigen (PSA) blood test, a screening tool used for prostate cancer in some European countries.
The study found that these PSA tests had little impact on reducing the number of deaths and, in some cases, did not detect some aggressive cancers early.
The results also indicated that these tests caused worrying rates of overdiagnosis in patients.
The study found that these PSA tests had little impact on reducing the number of deaths and, in some cases, did not detect some aggressive cancers early (file image)


The results also indicated that these tests caused worrying rates of overdiagnosis in patients (archive image)
Researchers from the universities of Bristol, Oxford and Cambridge invited more than 400,000 men aged 50 to 69 for screening, and just over half received a PSA test.
They followed these same men for 15 years and found that almost seven out of every 1,000 in the group who were invited to the test had died of prostate cancer.
This compares with almost eight men in every 1,000 who had not had a PSA test.
The trial results showed that about one in six cancers found by the single PSA test were an overdiagnosis that led to unnecessary treatment for tumors that were actually harmless.
Prostate cancer treatment can cause physical side effects, such as bladder and bowel problems, erectile dysfunction, and, in some rare cases, an infection after a biopsy.
The results showed that about one in six cancers found by the single PSA test were an overdiagnosis that led to unnecessary treatment for tumors that were actually harmless (file image).


Treatment for prostate cancer can cause physical side effects such as bladder and bowel problems, erectile dysfunction and, in some rare cases, an infection after a biopsy (file image)
Professor Richard Martin, lead author and Cancer Research UK scientist at the University of Bristol, told the Telegraph: ‘The key conclusion is that the small reduction in prostate cancer deaths by using the test to screen healthy men does not outweigh the potential harms.
‘This results in some men receiving invasive treatment they do not need, many years earlier than without screening, and the test also fails to detect some cancers that do need to be treated.
“We need to find better ways to detect aggressive prostate cancers, so we can treat them early.”
Prostate cancer claims 12,000 lives a year, making it the second leading cancer killer in men in the UK, the first being lung cancer.
It is the most common cancer in the UK without a screening programme, even though it often shows no symptoms until it spreads and becomes terminal.
The UK National Screening Committee (NSC) currently does not recommend prostate cancer screening because it is not clear whether the benefits of screening outweigh the harms.
Dr Neil Smith, Cancer Research UK GP and CEO of the Lancashire and South Cumbria Cancer Alliance, said: “With prostate cancer causing 12,000 deaths in the UK each year, we completely understand why men want know if they have the disease, even when they have no symptoms.
‘However, this research highlights that a PSA test for early detection may do more harm than good; It’s just not accurate enough and can lead some men to undergo tests and treatments they don’t need.
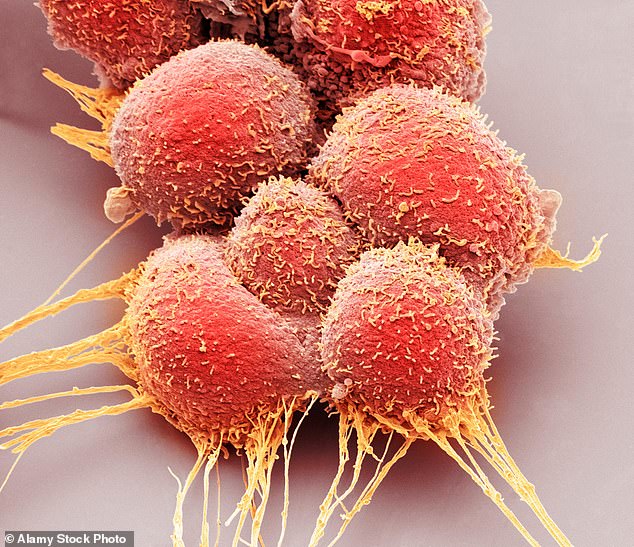
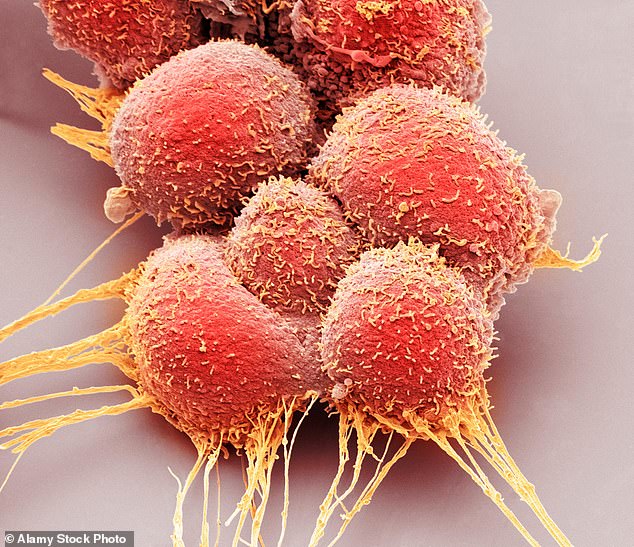
Prostate cancer claims 12,000 lives a year, making it the second deadliest cancer in men in the UK (archive image of prostate cancer cells)


Prostate cancer is the most common cancer in the UK without a screening programme, even though it often shows no symptoms until it spreads and becomes terminal (file image)
‘You know your body best, so if you notice any unusual changes, contact your GP. It’s probably not cancer, but if it is, catching it earlier means treatment will be more likely to be successful.’
In 2023, Prostate Cancer UK launched the £42m Transform trial, which aims to find out if MRIs are better for early detection.
Other clinical trials, such as STAMPEDE, are trying to find the best treatment for advanced prostate cancer to improve survival rates and quality of life.
Dr Matthew Hobbs, research director at Prostate Cancer UK, said: “A previous trial showed that screening with PSA blood tests reduces deaths from prostate cancer, but also misses important cancers and harms men who receive treatments or biopsies. There’s no need.
“The results from the UK CaP trial are extremely significant because they support these findings.
“The number of men screened who still died from prostate cancer in both trials makes it abundantly clear that the imperative now is to develop, test, and test new ways to diagnose prostate cancer that detect those aggressive cancers that PSA tests miss and reduce potential damage even further.’
