Chemicals used to protect your smartphone from fire may increase your risk of a deadly cancer, a study suggests.
Polybrominated diphenyl ethers (PBDEs) have been used since the 1970s for their ability to slow the spread of a fire, which could help save thousands of lives.
But now, in a study that followed 1,100 American adults for two decades, researchers found that those with the highest levels of these chemicals in their blood were four times more likely to die from cancer than those exposed to the lowest amounts. .
In particular, thyroid cancer was the most common, which has a survival rate of less than four percent if detected in the late stages.

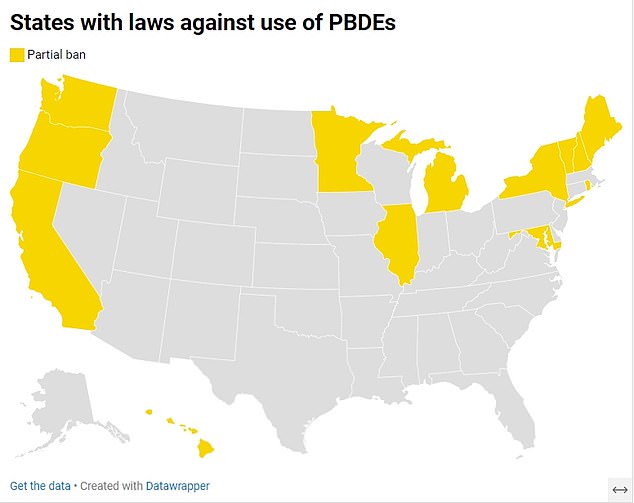
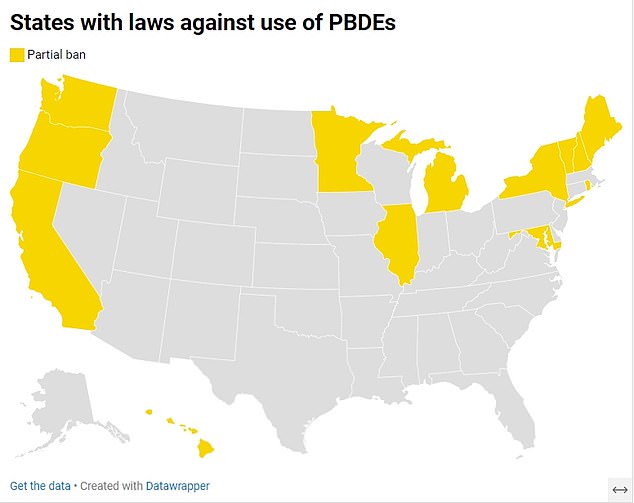
The map above shows states that have banned some forms of PBDEs. They are banned in many countries, including the European Union.
The Chinese scientists who carried out the research warned that PBDEs can break off from objects and form dust.
These can then enter humans through inhalation or as contaminants in food, disrupting hormones and damaging genes, increasing the risk of cancer.
TO 2017 study which tested 64 cell phones and PCs, from manufacturers such as Apple, Samsung and Dell, found that 60 percent had PBDEs on their surfaces. Apple says it no longer uses the chemical in its smartphones.
The flame retardant chemical is also found in other items, including sofas, chairs, car seats and children’s toys.
Many countries, including those in the European Union, have already banned or drastically limited the use of these chemicals.
But in the United States only 13 states, including New York, California and Maine, have imposed bans. Even then, only certain types of chemicals are restricted.
The scientists wrote in the article: ‘As (hormone-disrupting) chemicals, PBDEs and their metabolites can bind to hormone receptors (i.e., estrogen receptors)… and then disrupt hormonal homeostasis.
“This influences the development and progression of endocrine tumors such as thyroid cancer.”
The study also found that participants with the highest levels of the toxin in their blood had a 43 percent increased risk of all-cause mortality, meaning death from any cause.
But they said this was not a significant association and more research was needed.
The researchers said their study was the first to examine the link between PBDEs exposure and the risk of mortality from specific causes, including cancer.
For the study, researchers recruited participants from the National Health and Nutrition Examination Survey (NHANES) in the US, which surveys 5,000 adults and children each year.
Participants were recruited from the survey conducted in 2003 and 2004. They had an average age of 42 years and each had blood test results for PBDEs.
Each was then tracked for 17 years with records verified for death and cause of death.
During the study period, 199 participants (or 18 percent of participants) died.
The team then did an analysis adjusting for factors such as age, sex, ethnicity and obesity status.
The results revealed a 300 percent higher risk of cancer mortality among those with the highest levels of toxin in their blood compared to those with the lowest risk.
It also showed that those with the highest levels of the chemical had an eight percent lower risk of mortality from cardiovascular disease compared to those with the highest levels.
The study could only detect associations, but could not prove that the chemicals had caused the increase in cancer cases.
However, previous studies also warned about the risks of the chemicals, including that they could cause obesity in children.
The team, which examined thousands of cases, found that the chemicals could affect thyroid hormone levels and cause inflammation in pregnant women, leading to high birth weight and premature birth.
