Middle-aged women who sleep less than five hours each night are up to 75 percent more likely to suffer heart failure or stroke, a new study suggests.
Scientists at the University of Pittsburgh tracked nearly 3,000 women ages 42 to 52 over 16 years.
Every year for nearly two decades, women completed surveys about their sleep, including how many hours they slept on average each night and whether they considered themselves to suffer from insomnia.
They also completed health questionnaires to keep track of any ongoing illnesses or problems.
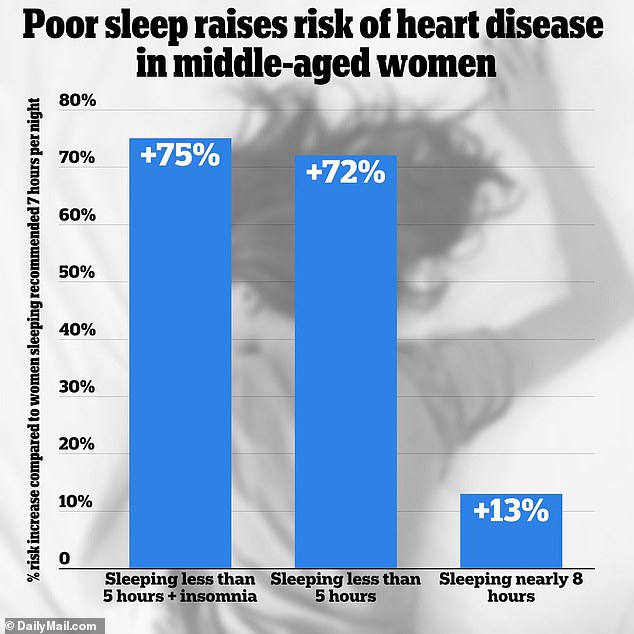
Analysis of the data revealed that women who regularly slept less than five hours a night were up to 75 percent more likely to suffer from a range of cardiovascular problems, including strokes, heart attacks, heart failure and coronary artery disease. .
Surprisingly, this relationship remained true even when other potentially contributing factors, such as BMI and underlying health conditions, were taken into account.
Scientists said this may be because getting too little sleep can raise blood pressure and trigger insulin resistance, increasing the risk of damage to blood vessels.
They also warned that it increased the risk of obesity, which is known to affect heart health, due to dysregulation of the body’s hunger and satiety hormones.
The graph above indicates that sleeping less than five hours per night increases the risk of heart disease in middle-aged women.

The data revealed that women who slept less than five hours a night were up to 75 percent more likely to suffer from heart problems.
The Center for Disease Control and Prevention (CDC) recommends that all Americans get between seven and nine hours of sleep each night.
But surveys suggest that one in three adults regularly fails to achieve this goal.
Among middle-aged women, surveys suggest that about half do not get the recommended seven hours of sleep each night.
Women in this age group are already at higher risk of heart disease. The drop in estrogen levels after menopause can cause blood vessels to become stiffer, cutting off blood flow to the heart.
The study, published in the journal of the American Heart Association CirculationUSD data from the Study of Women’s Health Across the Nation (SWAN), which followed thousands of women for 22 years.
She recruited premenopausal women ages 42 to 52 in 1996 and then followed them for the next 16 years.
During the study period, 200 cardiovascular events were reported, of which 23 resulted in death.
Cardiovascular events were defined as mycardial infarction (or heart attack), heart attacks, or receiving treatment for coronary artery disease.
About 10 percent reported having trouble falling asleep every night, while a quarter said they woke up several times during the night.
A total of 363 (or 14 percent) reported that they slept less than five hours each night on average, while 760 (or 30 percent) said they slept more than eight hours per night.
Most women (1,395 or 55 percent) reported sleeping about six hours and 30 minutes each night on average.
The researchers conducted an analysis adjusting for factors such as age, BMI, ethnicity, education, and underlying conditions.
They found that women who slept less than five hours a night on average were 72 percent more likely to suffer from heart disease than those who slept six and a half hours each night.
They also conducted a second analysis that also looked at reports of insomnia symptoms such as trouble falling asleep, waking up several times a night, or waking up earlier than expected.
It revealed that those who slept less than five hours a night on average and had insomnia symptoms more than three times a week were 75 percent more likely to suffer from heart disease.
They were compared to women who got the recommended amount of sleep and said they rarely suffered from insomnia symptoms.
The study authors, led by cardiologist Dr. Rebecca Thurston, wrote: “Symptoms of insomnia, when they persist through midlife or occur with short sleep, are associated with an increased risk of cardiovascular disease among women.”
Limitations of the study included that sleep duration and insomnia symptoms were self-reported and were not monitored by a medical device such as a smartwatch.
The researchers also did not consider other factors that affect sleep, including timing, regularity and efficiency, or how much light, deep and REM sleep a person had.
Cardiovascular disease is the leading cause of death among women in the US, and about 300,000 die from it each year.
More than 60 million women in the U.S. also live with some type of heart disease.