Cases of pancreatic cancer in young adults have skyrocketed in recent years but, to the confusion of scientists, deaths from this disease have not skyrocketed.
Now, a team of US experts may have discovered a possible reason.
Pancreatic cancer is considered one of the deadliest forms of the disease.
According to UK figures, fewer than one in 20 pancreatic cancer patients live to be a decade after their diagnosis.
Experts therefore expect to see a significant increase in pancreatic deaths in those under 50, to match the 2 to 8 percent increase in diagnoses over the past 18 years.
Experts now believe this has not happened because of the specific type of pancreatic cancer that affects young people, which is easier to detect and treat at earlier stages.
Pancreatic cancer is a general term for several tumors found in the 25cm tadpole-shaped organ that helps with both digestion and hormonal regulation.
One type, adenocarcinoma, is the most common, accounting for 90 percent of cases.
Becki Buggs was 43 when she received a devastating pancreas diagnosis and the nurse was motivated to get tested after her husband commented that she looked like “a Minion”, which was later revealed to be jaundice. Becki is shown here with her two children, Jacob and Georgie, who were 9 and eight years old respectively at the time.
This variant has few or no symptoms until patients suddenly begin to lose weight and turn yellow, at which point for the vast majority it is too late.
It is the reason why the disease has been called a “silent killer.”
But experts, led by doctors at Brigham and Women’s Hospital in Boston, found when analyzing the data that there was no increase in adenocarcinoma in young people.
Instead, the increase came from another type of pancreatic cancer, called endocrine cancer.
Unlike adenocarcinoma, these are slow-growing tumors that take decades to emerge, and while they can become cancerous, they are mostly benign.
Furthermore, the authors suspect that cancer does not actually appear more frequently in young people, but rather that doctors have much better tools to detect it.
They believe the increased use of high-tech medical scans such as CT scans and MRIs, which have become more sensitive over the years, are detecting more and more endocrine cancers.

Becki, now 45, knows she is one of the lucky few whose pancreatic cancer was detected early enough to be operable. It’s also part of a growing trend of younger women being diagnosed with the disease, a pattern that’s baffling experts.
These discoveries are often accidental: The scan does not target the pancreas itself, but rather doctors detect it while analyzing images while investigating another medical problem.
Dr. Gilbert Welch, a surgical and public health researcher at the Brigham and author of the study, published in Annals of internal medicinesaid The New York Times: “The more they imagine you, the more these things will appear.”
Despite guidelines that small endocrine tumors should be monitored with scans rather than removed with risky surgery, some doctors argue that they are better removed in younger patients.
They say that as younger patients live longer lives, there is more time for these cancers to eventually become deadly.
As Dr. Adewole Adamson, an expert on overdiagnosis at the University of Texas and co-author of the new study, explained, these requests for action are often driven by patients themselves.
“A lot of patients say, ‘Take it out,'” he said.
“When someone tells you that you have cancer, you feel like you have to do something.”
But doctors say the success of these types of interventions for endocrine cancer has not been evaluated.
Pancreatic cancer has been called a “silent killer” because of its subtle signs that are often detected too late.
Some are calling for endocrine cancer and the much more dangerous adenocarcinoma to be split so that the former is no longer classified as pancreatic cancer to help present data more accurately.
One Briton who has been affected by the devastation of a pancreatic cancer diagnosis is Becki Buggs, 46, from Colchester, Essex.
The first indicator that she had the disease was a casual comment from her husband, who told her she looked like a ‘Minion’, the yellow cartoon characters from the Despicable Me film series.
Looking in the mirror, the experienced nurse noticed signs of jaundice, yellowing of the skin and eyes and a serious indicator that something is terribly wrong with the body’s internal processes.
The mother-of-two had felt unwell on Christmas Day 2021, three days before the jaundice started, but suspected it was probably a Covid infection.
Rushing to the hospital for tests, he remembered that he strongly suspected it wouldn’t be good news.
‘Everything contributed to the fact that it was not going to be a good diagnosis. “It didn’t make it any easier,” he told MailOnline.
Three days later he received the devastating news that his fears were well founded: he had pancreatic cancer.
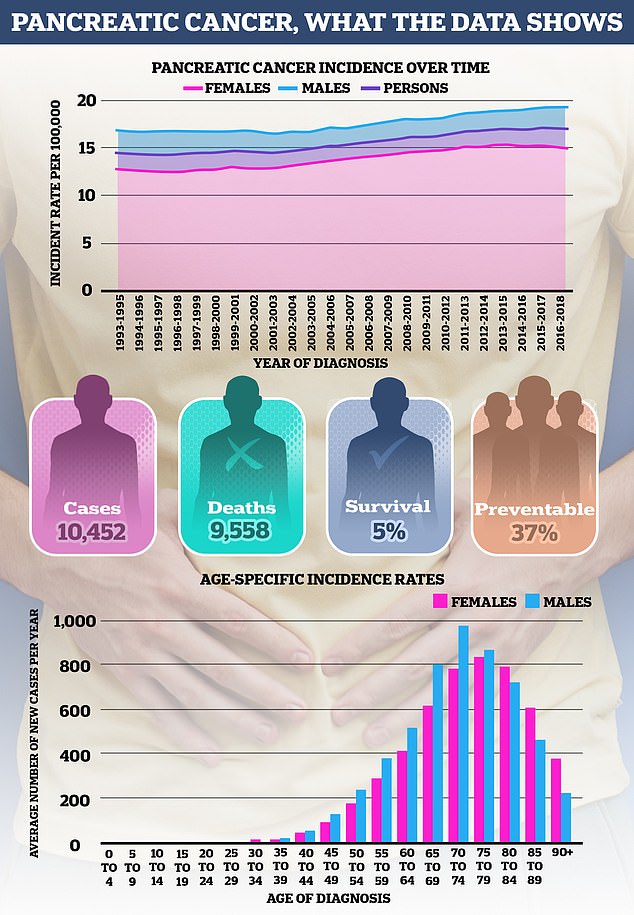
Pancreatic cancer remains one of the forms of the disease with the least survival and, worryingly, is on the rise. Data source: Cancer Research UK
Fortunately for her, she was one of the lucky few whose cancer was detected in its early stages, meaning she was able to undergo surgery.
He underwent a pancreaticoduodenectomy, also known as a Whipple procedure, a grueling operation in which cancerous tissue is cut out and then surgeons rearrange the patient’s digestive system.
Ironically, Becki had prepared pancreas patients for this procedure several times during her nursing career and described her own experience as the “toughest” test of her life.
“They were the hardest 11 days of my life,” he said.
‘It’s a horrible operation. There are no two ways to do it. It’s rewiring your entire digestive system, so it’s exhausting, but for me it wasn’t that bad because I knew what to expect.’
Becki, along with cancer experts, has urged people experiencing any of the subtle signs of pancreatic cancer to seek advice from their GP.
“I’m worried about other pancreatic cancer patients,” she said.
“It scares me that there are people who think, oh, I feel a bit unwell, but it’s okay, I won’t get a GP appointment, I’ll just tough it out.”
“Then they become so sick and jaundiced that they are admitted to the ER and by then it is too late.
“If you are concerned about any symptoms, please contact your GP.”
Pancreatic cancer kills around 10,000 Britons every year, roughly the equivalent of one death every hour in the UK.
Symptoms of pancreatic cancer include jaundice, where the whites of the eyes and skin turn yellow, along with itchy skin and darker urine.
Other possible signs include loss of appetite, unintentional weight loss, constipation, or bloating.
While the symptoms are unlikely to be cancer, it is important to get them checked early by a GP just in case, especially if people have had them for more than four weeks.


