Middle-class parents who normalize alcohol consumption are partly responsible for the high rate of underage drinking in England, experts suggested today.
One in three children has consumed alcohol by age 11 and one in two by age 13.
This is the highest rate of childhood alcohol consumption in 44 countries, according to a damning report commissioned by the World Health Organization (WHO).
Children from wealthy homes are the most likely to drink, with charities warning that they “mirror” the behavior of wealthy parents who frequently drink wine.
Pandemic-era restrictions that left children isolated and “stuck at home” could also be behind the surge seen in the wake of Covid, scientific commentators said.
The study, one of the largest of its kind examining data from more than 280,000 children, also showed that England has the highest levels of vaping in Western Europe at the age of 11.
By the age of 15, 40 percent of girls and a quarter of boys have tried e-cigarettes.
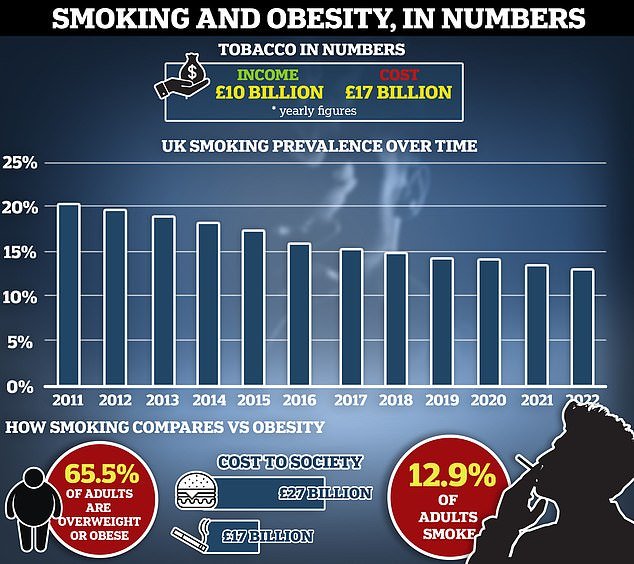
Smoking rates have also increased sharply.
Health chiefs have warned that more must be done to protect young people from these “toxic and dangerous products”, calling their use a “serious threat to public health”.
By the age of just 11, 34 per cent of girls and 35 per cent of boys in England have drunk alcohol, figures show – more than double the world average of 15 per cent.
At age 15, 56 percent of children from high-income families in England said they had drunk alcohol, compared to 39 percent from low-income families.
The gap was smaller among girls: 55 percent of those in rich areas had drunk alcohol, compared with 50 percent in poorer areas.
Dr Jo Inchley, international coordinator of the study, from the University of Glasgow, said this could reflect “cultural norms” among the middle classes.
He added: ‘Alcohol may be more normalized in wealthier families and, financially, may be more accessible.
“Alcohol is part of sporting culture in the UK, and young people from wealthy backgrounds are more likely to participate in sporting clubs and groups.”
Children also appear to be “initiating” alcohol consumption at a younger age, which may have accelerated during the pandemic, he said.
Dr Inchley added: “Part of this could be the effects of lockdown on social life, mental health and relationships with schools – we know Covid has had a huge impact on this group.”
In Scotland the figure was 16 per cent for girls and 17 per cent for boys. 14 per cent of girls in Wales and 20 per cent of boys have consumed alcohol by this age.
Under UK law, it is illegal to buy alcohol to anyone under 18 years of age. However, at ages 16 and 17, if accompanied by an adult, children can drink beer, wine or cider with a meal.
The NHS advises against drinking until the age of 18, warning that alcohol can damage children’s developing organs, including the brain and liver.
Dr Katherine Severi, chief executive of the Institute of Alcohol Studies, said: “People tend to have the perception that teaching children to drink in moderation is a good way to teach them safer drinking habits.”
‘This is false. The earlier a child drinks, the more likely they are to develop alcohol problems later in life.’
He added: ‘A pro-alcohol environment leads to the normalization of alcohol consumption and a “cultural blindness” to the harm of alcohol among children. This is true even when parents drink moderately.
“And as more well-off people tend to drink more, this normalization will be especially true, which likely explains why we see higher rates of alcohol consumption among children from well-off families.
“We know that children mirror the behavior of the adults around them, so it is important for parents who drink any amount to be aware of how it could affect their children in the future.”
Sir Ian Gilmore, president of the UK Alcohol Health Alliance, also blamed exposure to alcohol advertising for driving alcohol consumption at a young age.
He said it is “shocking” that children in the UK are more familiar with certain brands of beer than with biscuits, crisps and ice cream.
He added: “The government has introduced advertising regulations for other harmful products such as cigarettes and junk food – we urgently need a comparable approach for alcohol.”
The WHO survey covered young people living in Europe, Central Asia and Canada, and included more than 4,000 children in England.
It found that 40 per cent of girls and 26 per cent of boys in England had vaped by the age of 15, compared to a global average of 33 per cent and 31 per cent respectively.
Around 30 per cent of girls in England (almost one in three) have vaped in the last 30 days.
In England, more 15-year-old girls than boys have tried smoking (28 per cent compared to 16 per cent), and the rate among girls is higher than the world average (26 per cent).
Anne Longfield, chair of the Center for Young Life and former Children’s Commissioner, said: “We should be alarmed by the growing number of young people taking up vaping, our position at the top of the league for children’s alcohol consumption and its impact on health, development and the additional strain it will bring to the NHS.
“The Wild West era where vaping companies were allowed to do whatever they wanted must end.”
A government spokesperson said: ‘The health advice is clear: underage smoking, vaping and drinking can be harmful to young people and their development.
‘That is why there are age restrictions for the sale of these products.
‘As a Government, we are creating the UK’s first smoke-free generation.
“Our landmark tobacco and e-cigarettes bill will criminalize the sale of tobacco products to anyone born after January 1, 2009 and includes powers to limit flavours, packaging and displays of e-cigarettes to reduce their appeal for the children.”