A sex reassignment surgeon has unwittingly revealed the dangers of trans procedures, warning of poorly trained doctors leaving patients with dead appendages and other “feared complications”.
Dr. Alex Laungani, a physician at the Metropolitan Surgery Center of Canada, made damaging revelations about the “pretty bad” effects of sex reassignment operations while addressing colleagues.
The event, sponsored by the World Professional Association for Transgender Health (WPATH), was recorded and images were made public through a records request by the Daily Caller News Foundation.
Dr. Laungani joins a growing list of trans experts who, when speaking with like-minded professionals in clinical settings, are more candid about the downsides of trans care than is typically made public.
Dr. Alex Laungani is a surgeon at the Metropolitan Surgery Center in Montreal, Canada.

Her presentation, obtained by the Daily Caller News Foundation, included this slide about the post-op horrors of sex reassignment.
Dr. Laungani, his Montreal-based clinic and WPATH did not respond to our requests for comment.
Proponents of trans medicine say it saves lives among a suicide-prone group. Procedures to remove breasts and alter genitals help trans people live authentically, they say.
But critics warn of a cult-like trend, in which more and more trans people are “coming out” and undergoing risky procedures, while WPATH and other medical groups are hijacked by ideologues pushing reckless standards of care.
In the video, Dr Laungani warns of an explosion of more and more clinics serving increasing numbers of trans patients, where there is often “a lack of training and inadequate training”.
This massive rollout gave trans patients “access to surgery,” but at the cost of quality care, he said.
“It’s time to make sure we have the right training,” he said, calling for more scholarships.
Some doctors performed trans operations so infrequently that they were not “competent,” he warned.

Creating a neovagina is fraught with postoperative complications
They could mess up procedures and leave patients with “complications,” he added.
Dr Laungani said the results of delicate male-to-female genital surgeries, known as vaginoplasties, “can be quite bad”.
“The most feared complication is perforating the rectum while dissecting the vaginal cavity,” he added.
“You’re very close to the rectum and it’s very hard,” he said.
Reconstructing the area involves using meat from the “abdomen, scrotum or colon,” Dr. Laungani said.
Using tissue from the intestines has the highest risk of “complications,” he said.
Patients have problems after surgery, he said. Surgical wounds are reopened in three quarters of cases.
Afterwards, many patients cannot reach orgasm, he said.
Many have to “dilate” their newly created vaginal canals with a vibrator-like device to prevent them from collapsing.
It’s “what patients call a full-time job for the first few months, because it’s four times a day,” he said.

Dr. Laungani studied at the University of Liège in Belgium and worked at the renowned Mayo Clinic in Rochester, Minnesota.
One slide from her presentation describes other postoperative horrors, including “rectovaginal fistula, pelvic floor dysfunction, and clitoral necrosis,” when the sexual organ weakens and dies.
Laungani’s presentation was part of an educational series recorded in September 2022 for physicians seeking certification from WPATH, a world’s leading authority on gender-affirming care, as it is known.
WPATH is increasingly criticized for promoting trans procedures that critics say are experimental, dangerous and performed on patients who only need counseling.
Procedures are a hot topic in America’s culture wars, especially those affecting children.
The surgical alteration of the male and female genitalia to match those of the opposite sex (known as vaginoplasties and phalloplasties) is widely understood to be difficult and problematic procedures.
Women transitioning to become men may choose to construct a penis from tissue taken from their arms, although this procedure is also complex and the result is still markedly different from that of a biological penis.
Dr. Blair Peters, a pink-haired plastic surgeon at Oregon Health and Science University, has tens of thousands of followers on social media.
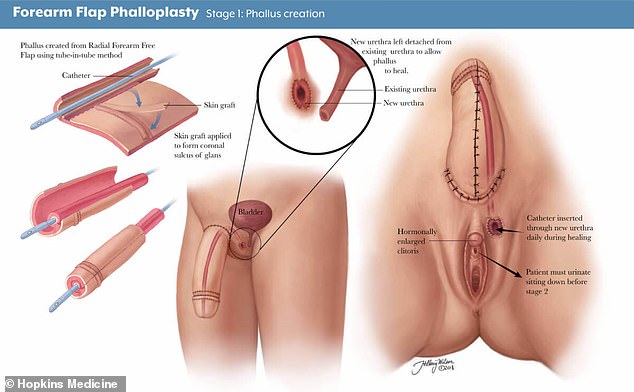
A phalloplasty procedure, as described in a medical textbook.
Removing the breasts of women transitioning from female to male is easier, but it can also cause pain, infections and problems such as stitches breaking, especially in overweight patients.
Dr Laungani’s video is just the latest example of a trans expert telling uncomfortable truths about his lucrative multi-million dollar business.
Marci Bowers, a male-to-female transitioning surgeon and president of WPATH, revealed how puberty blockers left trans children and teens unable to experience orgasms while speaking to her colleagues.
“I mean, it’s really about zero,” he said at a Duke University seminar in 2022.
Dr. Blair Peters, a plastic surgeon at Oregon Health and Science University (OHSU), revealed how trans children face a life of infertility, incontinence and sexual misery after surgery.
In a video interview with a colleague, Dr. Peters said the techniques were still being refined and “we’re learning and finding out what works.”
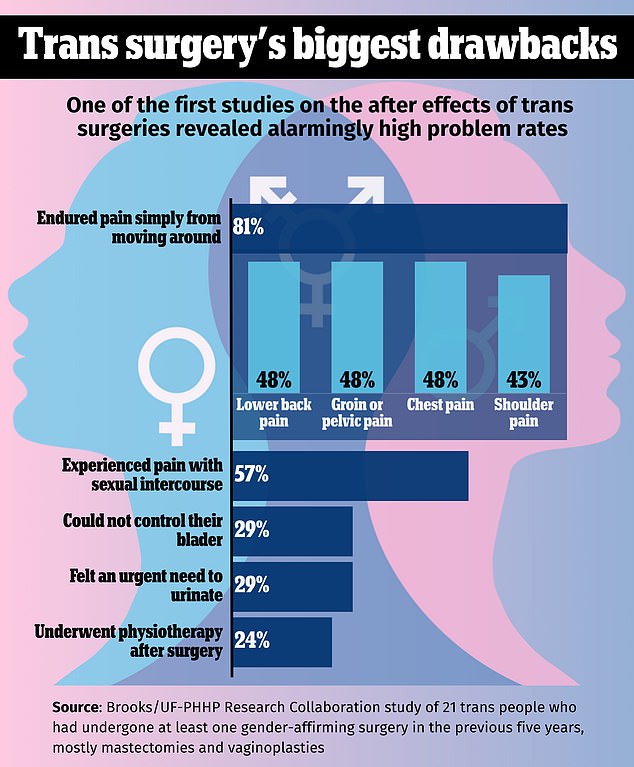
Most patients recovering from sex reassignment surgery experienced pain during sexual intercourse
One of the first studies on the side effects of transgender surgeries revealed alarmingly high rates of postoperative pain, pain during sex and bladder problems, raising troubling questions for this new frontier of medicine.
A large majority (81 percent) of those who underwent gender-affirming surgery in the past five years said they endured pain simply from moving in the weeks and months after going under the knife.
Researchers from the University of Florida and Brooks Rehabilitation, a nonprofit health organization, showed that more than half of trans-operated patients suffered pain during sexual intercourse and almost a third could not control their bladder.
Proponents of trans medicine present the surgeries as a trade-off, acknowledging the significant drawbacks but saying they are vital for those who have serious discomfort with their own bodies.
Still, they are rare within the transgender community.
Of the approximately 1.6 million trans and nonbinary Americans ages 13 and older, only 31 percent take cross-sex hormones and 16 percent opt for surgery, according to research by the Washington Post and KFF, a nonprofit organization. health.
Most surgeries are breast removals for people transitioning from female to male.


