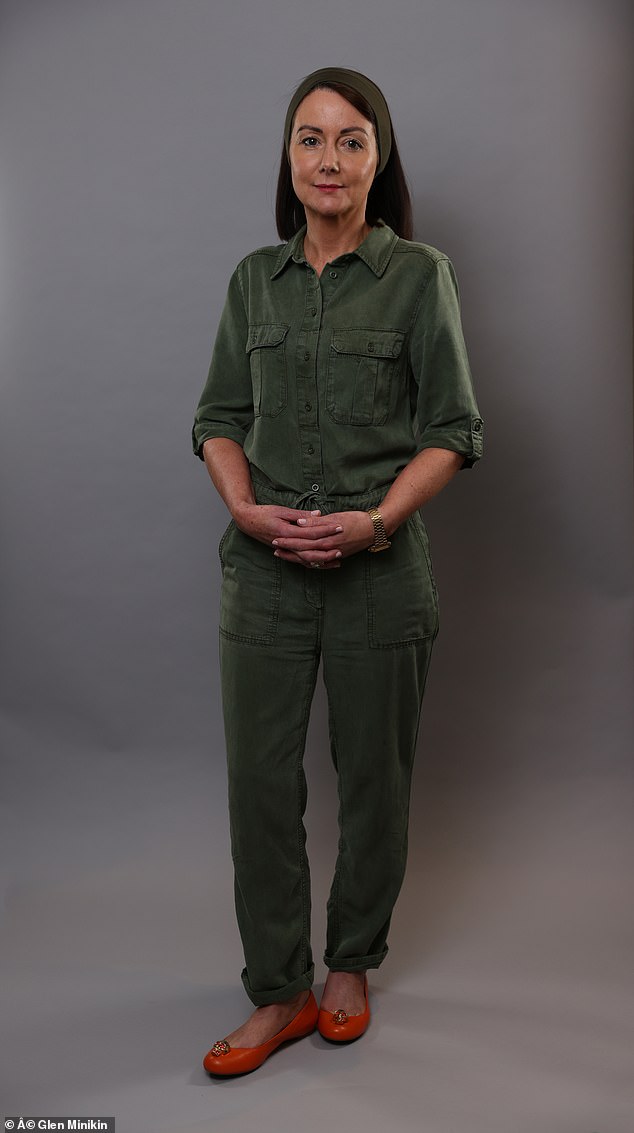
Every year, more than 12,000 people in the UK are diagnosed with brain tumours. Sarah Scanlan, 48, an oncology dietitian from Manchester, was one of the first to benefit from a new treatment that has fewer side effects, as she tells Adrian Monti…
The patient
While at my parents’ house in May of last year, I got up in the night to get a glass of water and suddenly discovered that I couldn’t breathe or speak.
I felt my eyes roll back in my head and I lost feeling in my right side before I fell to the kitchen floor, unconscious.
I don’t know how long I was unconscious, but when I woke up, I went to bed without telling my parents.
The next day I went to see my GP, who referred me as a non-urgent case to the hospital for an epilepsy test and told me not to drive for the moment.
I tried not to worry but a week later, in bed, I passed out again.
This time, when I regained consciousness, I went straight to the ER and had several tests done, including a brain MRI.
A few hours later they told me I had a brain tumor called a glioma.
On the positive side, it was benign; but it could mutate into a cancerous tumor, so it needed to be removed.
Sarah Scanlan, 48, an oncology dietitian from Manchester, was one of the first to benefit from a new proton beam therapy treatment for her brain tumor which has fewer side effects.

The purpose of the clinical trial that Sarah was invited to try was to see if the proton particles were as effective at shrinking the tumor as radiotherapy, while at the same time being less harmful to the surrounding healthy brain tissue (file image)
I was in shock, I felt like I had a time bomb inside my head.
I was put on daily pills to stop the seizures (caused by pressure from the tumor) and referred for surgery to remove as much of the growth as possible.
He would be awake during the operation as the tumor (the size of a golf ball) was close to parts of the brain that control speech, language and movement.
When I was awake, the surgeons could talk to me to check that these functions remained intact.
After a local anesthetic, I was operated on in a sitting position with my head in a kind of clamp to keep it still.
It took me seven hours and left me with a 10-inch scar on my head. However, my neurosurgeon said they had removed all but a small portion of the tumor.
The biopsy confirmed that it was an oligodendroglioma, a low-grade (i.e., slow-growing) tumor.
Additional treatment with radiotherapy and chemotherapy was necessary to control what was left.
But before that started, I was told I was eligible for a clinical trial at Christie Hospital, where I work, comparing proton beam therapy with standard radiotherapy.
Proton beams are a type of radiotherapy but are more precise than the usual method.
The purpose of the trial was to see if proton particles were as effective at shrinking the tumor as radiation therapy, while at the same time being less harmful to surrounding healthy brain tissue (especially areas involved in cognitive function and memory loss). ).
My first treatment was in March. I was fitted with a custom-made plastic mesh mask to ensure the rays hit their target.
The treatment lasted about ten minutes and I had 30 proton beam sessions every weekday for six weeks.
They left me tired and nauseous and I lost a lot of hair, but my cognitive function and memory have been fine so far. I also started chemotherapy last month.
I feel like I’ve wasted a year of my life, so next year, when I turn 50, I’m planning vacations, including Mexico.
I am a keen runner and hope to run the Manchester Marathon for The Christie Charity and give something back.
I feel lucky to have been chosen for this trial and I want others to benefit as well.
The specialist
Dr Gillian Whitfield is a Consultant Clinical Oncologist at The Christie NHS Foundation Trust in Manchester.
There are more than 130 different types of primary brain tumors (that is, tumors that start in the brain, rather than spreading from other places). In adults, a significant proportion belong to the group called gliomas.
Grade 1 and 2 gliomas are classified as noncancerous; The fastest growing grade 3 and 4 tumors are considered malignant.
For many, surgery is the first treatment, followed by radiation therapy, chemotherapy, or both.
The goal of surgery is to remove as much of the tumor as possible safely.
But that’s not possible for a tumor that has infiltrated vital parts of the brain (this could cause life-threatening lesions) or traps cells too small to be seen.
Radiotherapy aims to prevent visible and invisible tumor tissue from growing back.
Conventional radiation therapy uses x-ray beams to destroy cancer cells. This was usually done by illuminating rays from three or four directions.
Now, with more modern machines we can focus the X-rays more precisely and vary the intensity.
And more refined radiation therapy planning software means there is less damage to healthy tissue during treatment.
But even minor damage to healthy brain tissue from radiation therapy can mean long-term problems with memory and difficulty processing information.
With proton beam therapy, beams of particles called protons treat the tumor but, unlike x-rays, do not continue traveling (through healthy tissue) after reaching their target; instead, they stop.
This is expected to cause fewer long-term brain side effects, but to find out, we are part of the APPROACH trial with the University of Leeds.
246 patients participate in this trial; Sarah was our first recruit. Half will receive conventional radiotherapy and the other half will receive proton beam.
We target patients with oligodendroglioma.
There are around 350 cases a year in the UK and, although they are not as aggressive as a grade 4 tumour, they can cause death as they interfere with vital brain functions.
We know that patients who suffer from it usually respond well to treatment and the prognosis is good, with an average survival of more than 15 years; some patients live 30 or 40 years and may die with it rather than from it.
But cognitive problems, such as memory problems, can develop years after radiation treatment. And about half of all patients suffer from them as a result of radiation therapy.
However, all patients with oligodendroglioma will need radiation therapy at some point, as the benefits far outweigh the risks.

More refined radiation therapy planning software means there is less damage to healthy tissue during treatment. But even minor damage to healthy brain tissue from radiation therapy can mean long-term problems with memory and difficulty processing information.
Depending on the trial’s findings, patients with other brain tumors may also be eligible for proton beam treatment.
Those randomly selected will have a six-week course of 30 treatments if they have grade 2 oligodendroglioma; those with a grade 3 will receive 33 treatments over six and a half weeks.
Before starting radiotherapy, each patient will undergo neurocognitive testing, repeated one month after treatment and then annually for five years.
This trial will run for five years, and although we think proton beam therapy is likely to cause fewer neurocognitive problems, it will hopefully tell us whether that is the case.