OJ Simpson, the former football star and Hollywood actor whose trial for his ex-wife’s murder became a national sensation, died Thursday at the age of 76 after a brief battle with cancer.
Simpson became one of the greatest running backs in the history of college and then professional football.
His career began at the University of Southern California, where he received the Heisman Trophy in 1968 after setting the NCAA single-season rushing record.
He was then drafted first overall by the Buffalo Bills, for whom he played nine seasons, before concluding his career with the San Francisco 49ers.
In 1995, Simpson was acquitted by a Los Angeles jury of the murders of his ex-wife and her friend in what was called “the trial of the century.”
OJ Simpson, NFL Hall of Famer and many other things, died Thursday at age 76
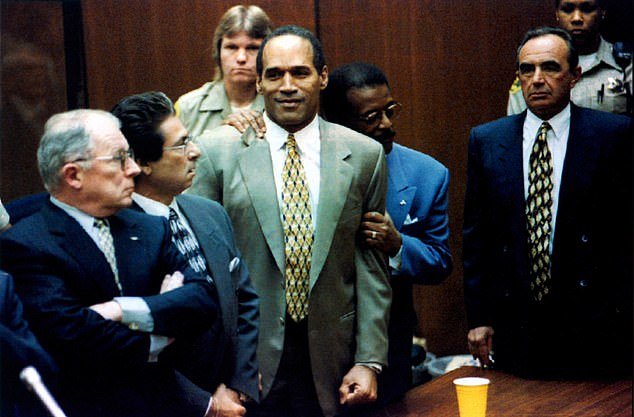
In 1995, Simpson was acquitted by a Los Angeles jury of the murders of his ex-wife and her friend in what was called “the trial of the century.” Here he is shown with his ‘dream team’ of defense lawyers.
He avoided prison when he was found not guilty of the 1994 stabbing deaths of his ex-wife Nicole Brown Simpson and her friend Ronald Goldman in Los Angeles.
He later served nine years in a Nevada prison after being convicted in 2008 of 12 counts of armed robbery and kidnapping at gunpoint two sports memorabilia dealers at a Las Vegas hotel.
Nicknamed ‘The Juice,’ Simpson was one of the best and most popular athletes of the late 1960s and 1970s. He overcame a childhood illness to become an electrifying running back at the University of Southern California and won the Heisman Trophy as the best college football player.
After a record-breaking NFL career with the Buffalo Bills and San Francisco 49ers, he was inducted into the Pro Football Hall of Fame in 1985.
Simpson parlayed his football stardom into a career as a sports commentator, publicist and Hollywood actor in films such as the ‘Naked Gun’ series.
That all changed after Nicole Brown Simpson and Goldman were found fatally stabbed in an incredibly bloody scene outside their Los Angeles home on June 12, 1994.
Simpson quickly emerged as a suspect. He was ordered to surrender to police, but five days after the murders, he fled in his white Ford Bronco with a former teammate, carrying his passport and a disguise.
A low-speed chase through the Los Angeles area, during which the former NFL player was driving a white Ford Bronco, ended at Simpson’s mansion and he was later charged with the murders.
What followed was one of the most notorious trials in the United States of the 20th century and a media circus.

Simpson became a football star while at USC, where he won the Heisman Trophy in 1968.
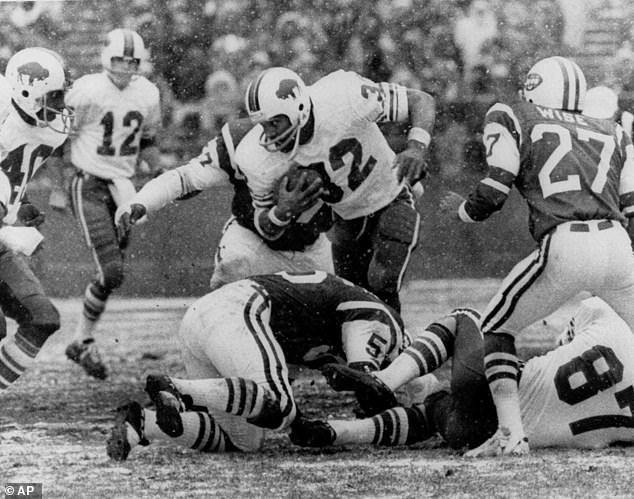
In this Dec. 16, 1973, file photo, OJ Simpson (32) of the Buffalo Bills runs against the New York Jets in the first quarter of an NFL football game at Shea Stadium in New York.
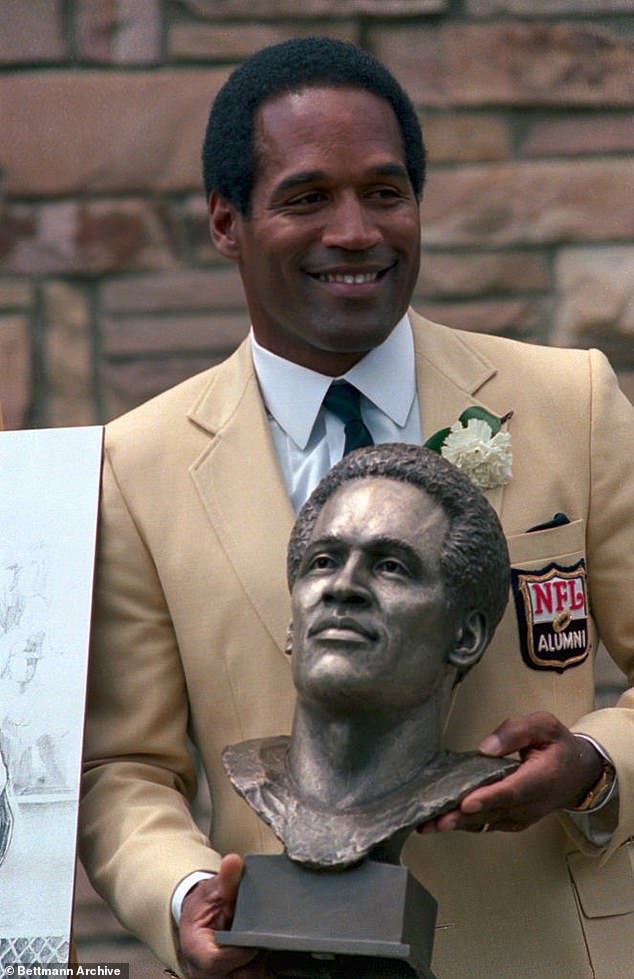
Simpson was enshrined in the Pro Football Hall of Fame in 1985.

Simpson turned to acting after his days in the NFL, starring in the Naked Gun films and appearing on television.
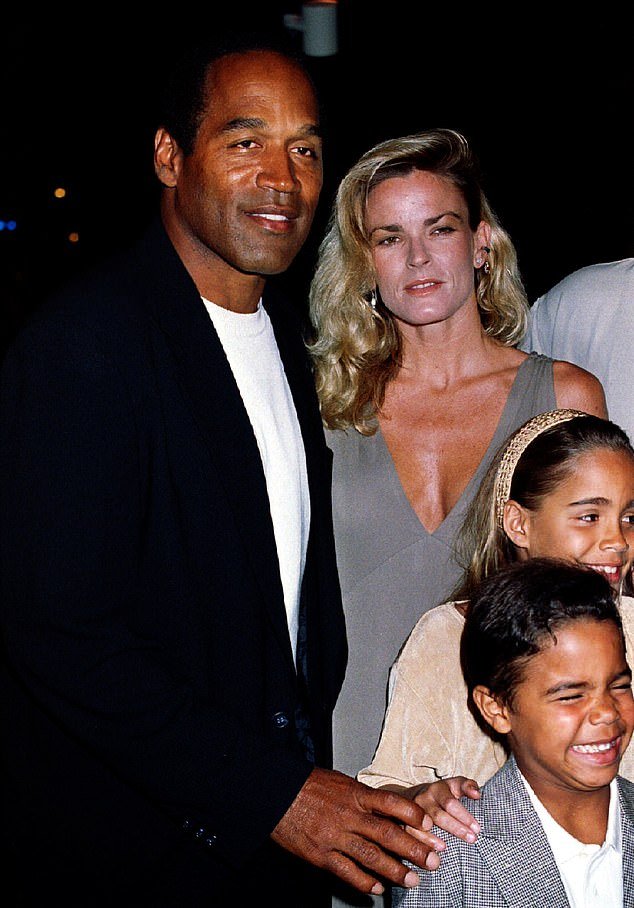
But his famous celebrity turned to infamy after the murder of his ex-wife Nicole Brown and her friend Ronald Goldman. Simpson was later arrested in connection with his murders.
He had it all: a wealthy, accused celebrity; a black man accused of killing his white ex-wife out of jealousy of him; a woman murdered after divorcing a man who had beaten her; a ‘dream team’ of expensive and charismatic defense lawyers; and a huge blunder on the part of prosecutors.
Simpson, who at the beginning of the case pleaded “absolutely 100 percent innocent,” greeted jurors and uttered the words “thank you” after the predominantly black panel of 10 women and two men acquitted him on Oct. 3, nineteen ninety five. .
Prosecutors argued that Simpson killed Nicole in a fit of jealousy and presented extensive blood, hair and fiber evidence linking Simpson to the murders.
The defense responded that the accused celebrity was framed by racist white police officers.
The trial paralyzed the United States. At the White House, President Bill Clinton emerged from the Oval Office and watched the verdict on his secretary’s television.

The crime scene where Nicole Brown and Ronald Goldman were murdered
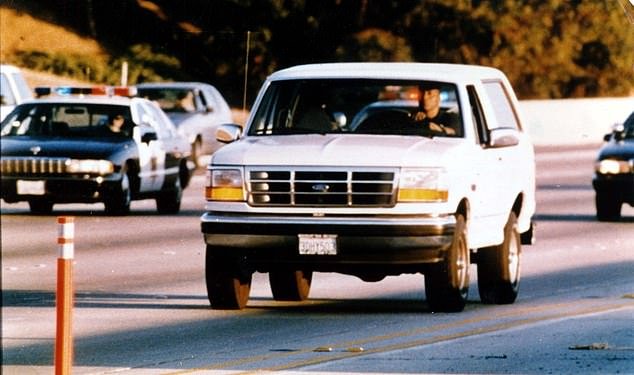
As police closed in on Simpson in the investigation, he led them on a long chase in a white Ford Bronco along the highways of Los Angeles.
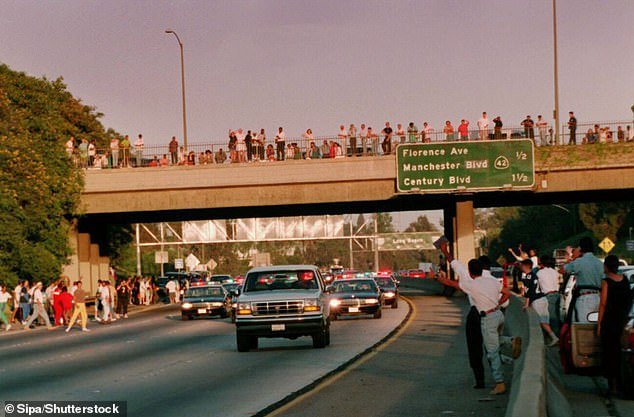
The police chase of OJ Simpson’s Bronco captivated the nation and brought people in Los Angeles to the streets to cheer on the NFL legend.
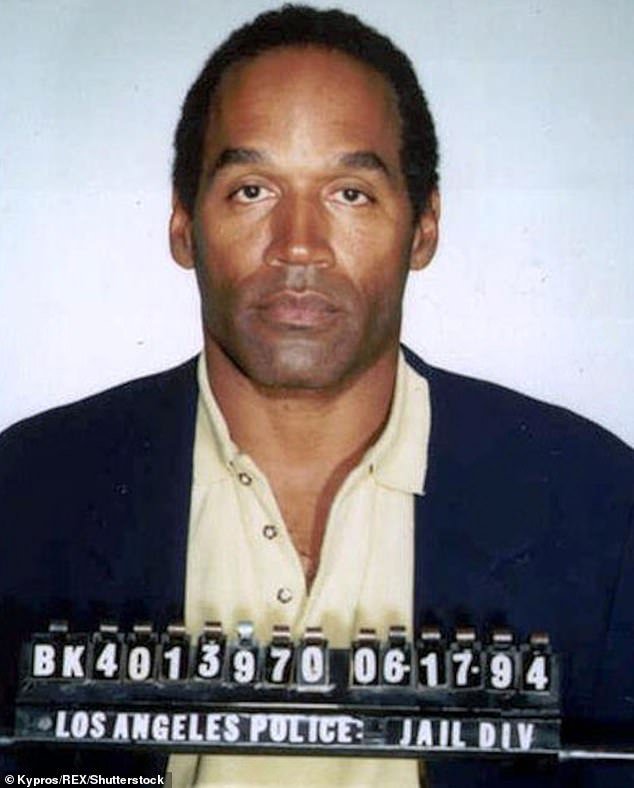
Simpson’s mugshot after his arrest

“If the glove doesn’t work, you must acquit,” became one of the most famous lines from the infamous Simpson trial.
Many black Americans celebrated his acquittal and saw Simpson as a victim of bigoted policing. Many other Americans were shocked by his exoneration in what seemed to have been an obvious victory for the prosecution.
The Goldman and Brown families subsequently filed a wrongful death lawsuit against Simpson in civil court.
In 1997, a predominantly white jury in Santa Monica, California, found Simpson liable for the two deaths and ordered him to pay $33.5 million in damages.
After the civil case, some of Simpson’s belongings, including memorabilia from his football days, were taken and auctioned to help pay for damages he owed.

On October 3, 2008, exactly 13 years after his acquittal in the murder trial, a Las Vegas jury found him guilty of charges including kidnapping and armed robbery. He was later sentenced to prison.

In recent years, Simpson has appeared frail while in Las Vegas.
On October 3, 2008, exactly 13 years after his acquittal in the murder trial, a Las Vegas jury found him guilty of charges including kidnapping and armed robbery.
They arose from a 2007 incident at a casino hotel in which Simpson and five men, at least two of them armed, stole sports memorabilia worth thousands of dollars from two dealers.
Simpson said he was just trying to get his property back but was sentenced to up to 33 years in prison.
“I didn’t want to hurt anyone,” Simpson said at his sentencing, dressed in a blue prison jumpsuit and shackled in leg and wrist shackles. “I didn’t know he was doing anything wrong.”
Simpson was paroled in 2017 and moved to a gated community in Las Vegas. He was granted early parole in 2021 due to his good behavior at age 74.