Thousands of patients with a common heart problem that leaves them weak and struggling to breathe are being denied a quick operation that could transform their lives and reduce their risk of death.
A life-threatening condition called mitral regurgitation (MR), which affects about one in 50 people, is caused by a leaky heart valve and can leave sufferers exhausted even during everyday activities such as showering or getting dressed.
Open heart surgery can fix the problem, but it is often considered too risky. But now surgeons have developed a keyhole procedure which they believe could treat thousands more MRI patients – but they say the NHS is blocking it.
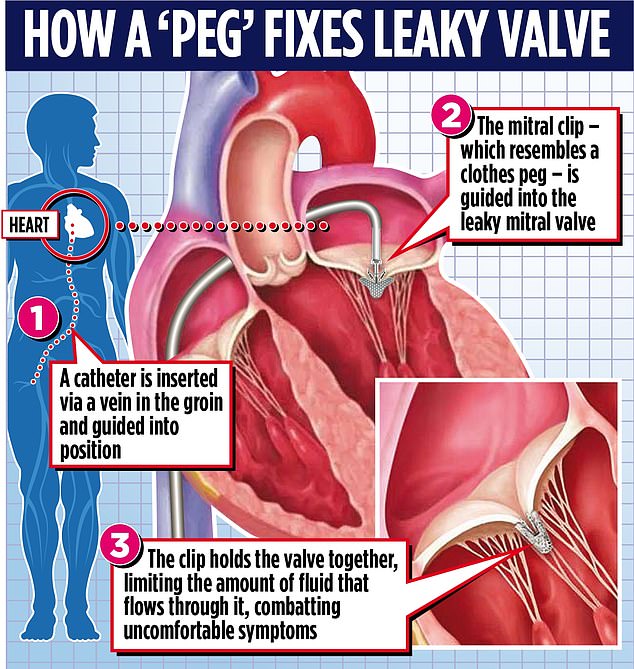
Called transcatheter edge-to-edge repair (TEER), this remarkable operation inserts a thin tube called a catheter into a vein in the patient’s groin to guide a small clip, like a clothespin, toward the heart.
Trimming the faulty valve can reduce the leak and restore normal heart function, dramatically improving the quality of life of even seriously ill patients. The procedure lasts two hours, has minimal recovery time and, being less invasive, reduces complications.
Called transcatheter edge-to-edge repair (TEER), the remarkable operation inserts a thin tube called a catheter into a vein in the patient’s groin to guide a small clip, like a clothespin, toward the heart.

A life-threatening condition called mitral regurgitation (MR), which affects about one in 50 people, is caused by a leaky heart valve and can leave sufferers exhausted even during everyday activities such as showering or dressing (file image )
But at a price of around £30,000 per patient, around double the cost of open heart surgery, the NHS has only authorized this relatively new procedure for a limited category of patients. That’s why activists are urging him to change the rules to make it more available.
Dr Jonathan Byrne, a consultant cardiologist at King’s College London and leader of the Valve For Life group in the UK, which aims to expand access to keyhole therapies for those suffering from heart valve diseases, warned that too many patients They were left suffering.
He said: ‘Large numbers of patients are excluded from this routine, safe and effective treatment. They continue to struggle with debilitating symptoms. They will need to see their GPs frequently. Many come and go from A&E. Some will even die.
“It’s very frustrating because TEER is actually very simple, even for a patient who is unwell.”
TEER brought Nicolae Olifirenco, 44, back to life after a heart attack. He was rushed to the hospital in the middle of the night, where he was diagnosed with severe heart failure and a leaky mitral valve.
Unlike a heart attack, which occurs due to a blockage in circulation, heart failure is a long-term fatal condition in which the muscle does not pump as well as it should, so not enough oxygenated blood circulates through the body. , resulting in debilitating symptoms. .
Olifirenco, struggling to breathe, was bedridden and so weak that he could not wash or change his pajamas without help. After a month in intensive care, he was warned that he might need a heart transplant.
While he was technically not eligible for TEER, the NHS decided to make an exception and offer him the procedure due to the severity of his condition.
Last month, Dr. Byrne performed the procedure, which allowed Mr. Olifirenco to return home and resume his normal life.
Olifirenco, a Ukrainian living in London, said: “The day I had a heart attack, I woke up at one in the morning with severe pain in my chest and left arm. I couldn’t breathe properly. My blood pressure I was very high and my body was swollen: my legs, arms, face.
‘He needed 24-hour surveillance and couldn’t even walk.

But at around £30,000 per patient, around double the cost of open heart surgery, the NHS has only authorized the relatively new procedure for a limited category of patients (file image)
‘He had a very leaky heart valve and was suffering from severe heart failure. I found myself in intensive care for about a month.
“I was so unwell that the team were considering an urgent heart transplant. I was terrified – I never thought I would leave the hospital.
“Fortunately, my doctor was able to offer me the keyhole mitral TEER procedure and I made a full recovery.”
The mitral valve is a small valve in the heart that ensures that blood flows in only one direction. Mitral regurgitation occurs when the valve does not close properly, so blood flows in the wrong direction.
MR affects approximately two percent of the population, although most are treated with medications, not surgery. The condition is more common in older people. A variant, degenerative MR (DMR), occurs when wear causes the valve to leak. Another, called functional MR (FMR), occurs when the valve does not work due to some other condition or problem, such as a heart attack or heart failure.

MR affects approximately two percent of the population, although most are treated with medications, not surgery. The condition is more common in older people (file photo)
Until recently, severe mitral regurgitation could only be solved by repairing or replacing the mitral valve through open heart surgery. However, such major surgery is too risky for some patients. Surgeons also found that although open-heart surgery is good for treating patients with DMR, it is less effective and riskier for patients with FMR.
In contrast, TEER works for patients with any of the MR variants and can even be used where open heart surgery would not be appropriate. But in 2019, the NHS stated that TEER could only be used for patients with DMR – around 500 a year.
Doctors believe it could also be offered to around 3,000 FMR patients a year.
Professor Dan Blackman, chair of the Structural Heart Group at the British Society for Cardiovascular Intervention, also believes it should be more widely available. He said: ‘TEER is standard in other countries, but we have the lowest rate in Europe. “I hope the NHS reconsiders.”
Last week, NHS England said it will re-examine the use of TEER for patients with FMR.
A spokesperson said: “NHS England is committed to commissioning safe and effective treatments for patients across all clinical specialties in a fair and equitable way.”