- 24 cases of infectious leptospirosis reported in New York City in 2023
- Between 2001 and 2020, the city recorded only three human cases a year.
- READ MORE: Arkansas man contracts virus carried by rats with 40% mortality rate
New York City has issued a health alert due to the increase in diseases transmitted by rats.
Cases of leptospirosis among people soared to their highest level in 2023, which is transmitted through contact with rat urine or feces.
In 2023, 24 cases were reported in the city, eight times more than the total number of cases in the previous two decades.
So far in 2024, there have been six cases.
“Rodents are not only unsightly and can traumatize your day, but they also represent a real health crisis,” saying Mayor Eric Adams.
Rat-related diseases reached their highest level in 2023, with 24 cases reported in the city
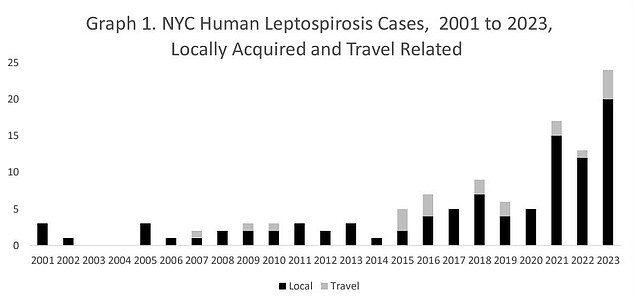
Between 2001 and 2020, New York City saw only three cases of human leptospirosis per year. That increased eight-fold in 2023. So far in 2024, there have been six cases.
When animals such as rats are infected with leptospirosis, they may not show symptoms of the disease.
But they may continue to shed bacteria into the environment continuously or occasionally for a few months to several years.
Humans can become infected through contact with the urine of infected animals.
The health alert, sent by the Deputy Commissioner of the Disease Control Division to his colleagues, said: “Twenty-four people diagnosed with leptospirosis were reported in 2023. This exceeds the total number of cases… of any previous year.”
“For comparison, the average number of locally acquired cases between 2021 and 2023 was 15 per year, and three cases per year between 2001 and 2020. This year, six cases have been reported as of April 10, 2024” .
Among the 98 locally acquired cases reported between 2001 and 2023, the median age of patients was 50 years. About 94 percent of the cases were men and most came from the Bronx.
Leptospirosis infections are not common in the US, with only 100 to 150 diagnosed each year, up to 15 percent of which are fatal.
Six people died from leptospirosis between 2001 and 2023 in New York City, according to the New York City Department of Health and Mental Hygiene.
New Yorkers are told to watch for symptoms such as high fever, headache, chills, muscle aches, vomiting, jaundice (yellow skin and eyes), and red eyes. Abdominal pain, diarrhea, and rash may also occur.
Authorities are concerned because infection often comes from handling garbage bags or containers with food waste, which a rat or other infected animal may have urinated on.
If left untreated, leptospirosis can lead to kidney failure, meningitis, liver damage, and respiratory distress.
Deputy Mayor Anne Williams-Isom said: “In terms of awareness, I understand, if we wear gloves, the supers or the people who tend to deal with large quantities of plastic bags.”
Mayor Adams is trying to remove trash bags from the street and place trash in containers.
Mayor Adams said, “If you opened your closet and a rat escaped, you would never open it the same way again.” “If you went to the bathroom and a rat crawled into your bathroom, you would never feel comfortable in that bathroom again.”

