A 39-year-old woman diagnosed with fatal stage four cancer said doctors dismissed her debilitating pain as “just a heavy period”.
Emma McQuitty, from north Belfast, went to A&E in February after suffering constant bleeding and pain that left her unable to walk.
But after 15 hours at the Mater Hospital, the mother of one boy says she was sent home with strong painkillers. On four further visits over the next six months she was also discharged and given co-codamol, she says.
It was only after the pain worsened in July that her worried family urged her to go to the Ulster Hospital, run by an independent NHS trust.
Emma McQuitty, from north Belfast, went to A&E in February after suffering constant bleeding and pain that left her unable to even walk. But after 15 hours in the Mater Hospital, she says she was sent home with strong painkillers. On four further visits over the next six months she was also discharged on co-codamol, she says.
There, doctors discovered she had stage four cervical cancer and that tumors that had formed in her cervix, uterus and bladder had spread to other parts of her body.
The single mother of one also says that as she prepared to receive treatment, she suffered kidney failure and life-threatening sepsis.
Recalling her ordeal, Ms McQuitty said: Belfast live‘I feel like if the doctors had listened to my concerns sooner, maybe I wouldn’t be in the horrendous situation I’m in now, having to undergo treatment for stage four cancer and multiple tumors.
‘I was going to A&E for six months and every time I was sent home with co-damol and the doctors told me I’d just had a heavy period, when in fact I needed urgent tests and treatment.
‘I am very grateful for the care I am now receiving at Ulster Hospital, which has gone above and beyond what I expected.
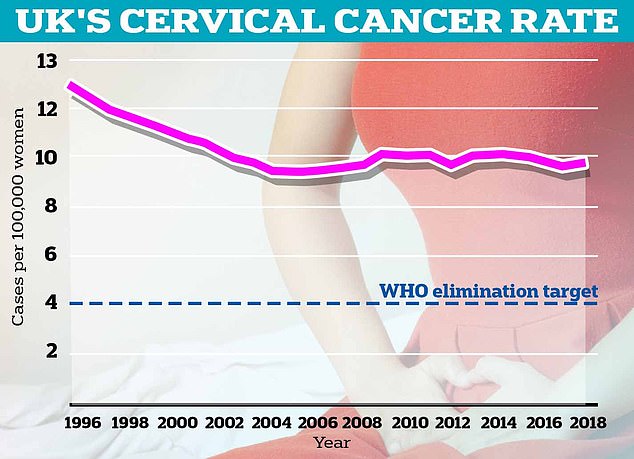
Technically, elimination would be achieved when fewer than four women per 100,000 are diagnosed (blue dotted line). By comparison, in England 9.5 women per 100,000 are diagnosed with cervical cancer (dotted line), which equates to 2,626 cases per year.
Cervical cancer symptoms to look out for include unusual vaginal bleeding, pain during sex, and lower back or pelvic pain.
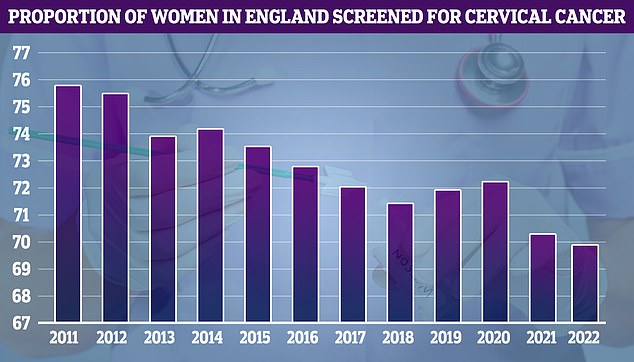
NHS cervical cancer screening data, dating back to 2011, shows uptake was at its highest that year (75.7 per cent) and has declined over time.
‘But I know that I have a very difficult road ahead of me with my treatment.
“My health has deteriorated so much that I can barely walk on my own and I need help to get anywhere. I wish they had listened to me from the beginning.”
Currently, around 3,000 women in the UK are diagnosed with cervical cancer each year, representing a decrease of around 25 per cent since the early 1990s.
It causes around 685 deaths each year in England.
But only 15 per cent of people diagnosed with stage four cervical cancer survive five years or more after diagnosis, Cancer Research UK says.
A combination of radiation therapy and chemotherapy is often offered in stage four to shrink the cancer, reduce symptoms, and help you feel more comfortable.
Surgery is usually only recommended if the cancer is causing a blockage in the kidneys or bowel, according to the charity.
Experts have credited the human papillomavirus (HPV) vaccine, which became available on the NHS in 2008, with helping to reduce the number of women affected by the disease.
However, the injection, like all vaccines, does not offer 100 percent protection.
Almost all cervical cancers are caused by infection with HPV, a common group of viruses that are transmitted through sexual contact and usually cause no symptoms.
Cervical cancer screening, offered to women aged 25 to 64, provides another form of defence against cancer by checking for changes in cervical cells caused by HPV.
If detected, these cells can be treated before they become cancer.
Ms. McQuitty’s daughter, Codie, and a friend have launched a GoFundMe to help cover the cost of a mobility scooter and other home devices to assist her during treatment.
Since its launch a week ago it has already raised more than £5,000.
Belfast Health and Social Care Trust has been contacted for comment.
Overall, the uptake rate for cervical cancer screening remains low in the UK. Only around 70 per cent of eligible women – around 4.6 million – attend a scheduled test.
Shame is a factor, according to research by cervical cancer charities.
This can be especially a problem for women from certain cultural backgrounds.
For half of the 1.3 million people who don’t show up each year, getting time off work and finding a convenient time to make an appointment are other reasons for not showing up.
Last month, however, NHS England revealed that women could soon be offered cervical cancer screening tests they can carry out themselves, after research found that self-administered tests at home significantly improved detection rates.


