A grieving sister has launched a legal battle against a hospital accused of keeping her brain-dead brother alive for years to boost his performance ratings.
Darryl Young, 61, suffered irreversible brain damage and was left in a vegetative state after a failed heart transplant procedure at Newark Beth Israel Hospital in New Jersey in 2018, according to a new lawsuit.
The lawsuit alleges that the center only kept Young alive to improve its transplant survival records, which had fallen below the national average after a pattern of failed surgeries.
Audio recordings obtained by ProPublica appeared to show hospital staff saying they would do everything they could to keep their patient alive to increase their survival rates even though there was no chance of recovery.
The alleged cover-up by hospital staff, which one doctor privately called “highly unethical,” came after damning government inspection reports found the facility put patients in “immediate danger.”
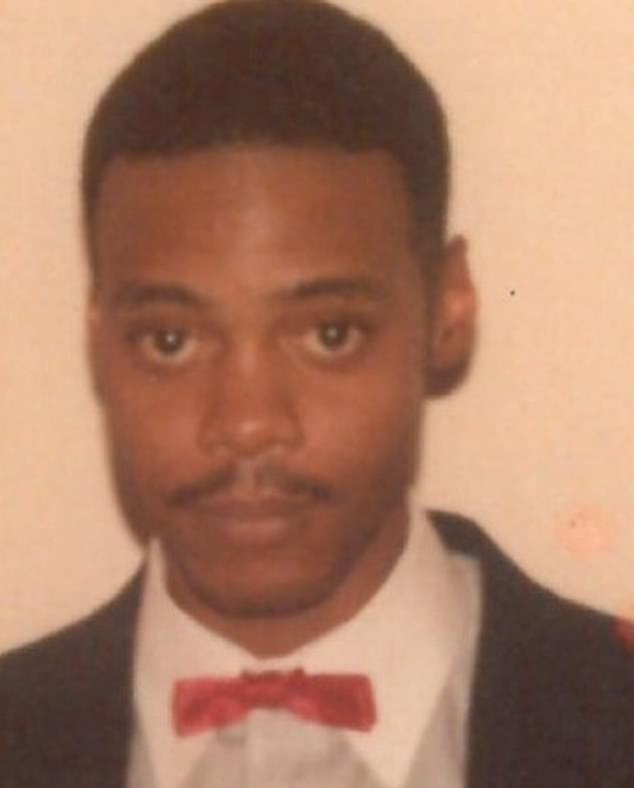
Darryl Young allegedly stayed alive for four years despite having extensive brain damage and no chance of recovery. The hospital hid the truth about his condition and poor prognosis from his family, the lawsuit claims (Photo courtesy of Mr. Young’s obituary)
The Centers for Medicare and Medicaid Services, which regulates hospitals that receive federal funds, like Newark Beth Israel, found in 2019 that the hospital failed to implement measures it deemed necessary to save patients.
He lawsuit against the individual doctors and the health center alleges that staff were “negligent and deviated from accepted standards of practice”, leading to Mr Young’s tragic outcome following a failed heart transplant.
Young, who needed a heart transplant for congestive heart failure, suffered brain damage believed to be due to a dangerous drop in blood pressure during surgery and showed no signs of regaining consciousness.
At first, Andrea Young’s family was told that the surgery had gone well and there was nothing to worry about. But as the days passed without her brother waking up, Mrs. Young became restless.
Dr. Margarita Camacho, the surgeon who performs the vast majority of heart transplants, including Young’s, assured him that she had seen patients recover from similar situations, according to the lawsuit.
Ms Young was later told her brother had brain damage, but only in small concentrations, which initially gave her sister hope.
She saying: “Now I know it was a false hope.”
Despite showing no brain activity, the lawsuit claims, doctors and nurses kept Mr. Young hooked up to a feeding tube for nutrients, suctioned mucus from his lungs and hooked him up to a respirator.
He remained alive until September 2022.
Mrs. Young said ProPública that while he understands that medical errors happen, “it is your duty and responsibility to be honest and let the family know exactly what went wrong.”
The struggle to learn about her brother’s condition and the deception of the hospital staff was so frustrating that she even read medical articles and textbooks in the library to know the right questions to ask.
He added: “I remember as clearly as if it were yesterday, my desperation for answers.”
Ms. Young hopes the lawsuit will hold the hospital accountable: “Especially since the doctors were never, from the beginning, forthcoming and honest about the circumstances of my brother’s condition, it is not only wrong and unethical, but it took a lot away from us.” our entire family.
“The most important thing for me is that those responsible are held accountable.”
While the hospital has not filed a response to Ms. Young’s legal complaint, spokeswoman Linda Kamateh said, “Newark Beth Israel Medical Center is one of the nation’s leading heart transplant programs and we are committed to serving our patients with the highest quality of care. . As this case is in active litigation, we are unable to provide further details.’
The high number of deaths after transplants (at least six) could partially explain why the heart transplant program’s one-year survival rate fell below 85 percent in 2018, according to ProPublica, well below average national around 89 percent.
The hospital performs around 29 heart transplants a year.
According to a report by ProPublica, the doctors who treated Mr. Young met in secret after the botched surgery on September 21, 2018, which caused the patient to suffer pneumonia, strokes, seizures and a fungal infection, although not it is clear what specifically caused each of them. of these effects.
They agreed that they should do everything possible to keep him alive, according to the investigation of ProPúblicato boost your survival rate.
In recordings of the meeting obtained by the news site, Dr. Mark Zucker, director of the hospital’s heart and lung transplant programs, said, “We need to keep him alive until at least June 30.”
The program’s survival rate had been falling for years. If it fell below a certain level designated by CMS (73 percent of patients survive after a year), it could trigger a federal audit.
If that audit uncovered serious problems, such as abnormally low survival rates, the hospital would no longer receive Medicare reimbursement for the transplants.
The hospital’s heart transplant survival rate would drop from 84.2 per cent to 81.6 per cent if Mr Young were the seventh patient to die.
While this would not warrant a formal audit, ProPublican reported that the transplant team was concerned that this decline would attract unwanted attention from the federal government.
According to the report, Dr. Zucker said: “If he is not dead in this (annual survival rate) report, even if he is dead in the next report, it becomes a problem that will extend six more months.”

Newark Beth Israel Hospital has not formally responded to the legal complaint, although a spokesperson maintained that “we are committed to serving our patients with the highest quality of care.”
Mr Young suffered brain damage during his heart transplant and never woke up. A doctor’s note about his condition after surgery said: “He is not following any orders. He appears very encephalopathic, meaning brain damaged.
Doctors are supposed to inform the patient’s family when an operation doesn’t go as planned and the patient doesn’t wake up. But Ms Young claimed they never had that conversation with her.
The hospital insisted on holding a family meeting with Mrs Young to discuss her brother’s condition. But, according to the judicial complaint, the medical team did not communicate the patient’s poor prognosis.
A follow-up on May 23, 2019 showed that Ms Young had yet to receive updates after a procedure was canceled due to her brother’s deteriorating condition. Medical records indicated a poor prognosis, but she was not informed.
She was also not informed that she had contracted a deadly fungal infection in the hospital called C. auris, which is resistant to many medications and can cause skin and bloodstream infections.
The lawsuit claimed that the hospital also corrective measures ignored in several other cases.
ProPublican found that in 2018, two patients, one who received a heart transplant and another who received a lung transplant, suffered kidney failure. The complication was linked to severe drops in blood pressure, which is also what caused Mr Young’s brain damage.
After the first incident, the hospital’s internal policy recommended increasing the frequency of blood pressure readings.
Then, after the second incident, the hospital again recommended better surveillance. CMS found no indication that staff implemented the new policy at that time.