“Miracle” weight-loss injections could help improve brain health and even reduce nicotine dependence, research suggests.
Semaglutide, the active ingredient in Ozempic and Wegovy, has been hailed as a monumental breakthrough in the war on obesity.
Now, British experts say the shots could also reduce the risk of cognitive decline, substance abuse and even encephalitis, compared with other diabetes drugs.
The researchers did not speculate why the drugs, which belong to a class of drugs called GLP-1 agonists, might help in this way.
Instead, they called the findings “significant” and said they could pave the way for new treatments, although they cautioned that more research was needed.
Semaglutide, the active ingredient in Ozempic and Wegovy, has been hailed as a monumental breakthrough in the war on obesity. Now, according to British experts, the injections could also reduce the risk of cognitive decline, substance abuse and even encephalitis, compared with other diabetes drugs.
Dr Riccardo De Giorgi, an expert in adult psychiatry at the University of Oxford and lead author of the study, said: ‘Our results suggest that the use of semaglutide could extend beyond the control of diabetes, potentially offering unexpected benefits in the treatment and prevention of cognitive decline and substance misuse.
‘Therefore, the findings of our study not only help to reassure the millions of patients who rely on semaglutide for the treatment of diabetes, but, if confirmed, could also have significant public health implications in terms of reducing cognitive deficit and smoking rates among patients with diabetes.’
Study co-author and expert in the treatment of psychiatric disorders at the University of Oxford, Dr Max Taquet, added: ‘Our study is observational and therefore these results should be replicated in a randomised controlled trial to confirm and extend our findings.
‘However, this is good news for patients with psychiatric disorders, who are at higher risk of developing diabetes.’
In the study, researchers followed more than 120,000 Americans with type 2 diabetes between 2017 and 2021.
During a one-year follow-up, they compared the risks of 22 neurological and psychiatric diseases among patients taking semaglutide versus those taking sitagliptin, a drug for type 2 diabetes.
A second cohort of semaglutide users was analyzed against empagliflozin and a third against glipizide. Both are also type 2 diabetes medications.
The 22 conditions evaluated include encephalitis, Parkinson’s, cognitive deficit, dementia, epilepsy, migraines, insomnia, nervous disorders, muscular diseases and intracranial hemorrhage.
These include, but are not limited to, ischemic stroke, alcohol abuse, opioid abuse, cannabis abuse, stimulant abuse, nicotine abuse, psychosis, bipolar disorder, depression, anxiety, obsessive-compulsive disorder, and suicidality.
Writing in the diary, eClinical MedicineThe scientists said: ‘Semaglutide was not associated with an increased risk of neurological and psychiatric outcomes.
‘In contrast, after correction for multiple testing, semaglutide was associated with a reduced risk of several of these outcomes.’
The greatest risk reduction was seen in encephalitis: patients treated with semaglutide were 74 percent less likely to develop the disease than those treated with glipizide and 65 percent less likely than patients treated with sitagliptin.
Semaglutide users were also 28 percent less likely to experience cognitive decline than those taking sitagliptin and glipizide.
Other significant reductions in dementia were seen, with a 48 percent lower chance compared with sitagliptin and 37 percent with glipizide.
Nicotine misuse was 28 percent less likely for glipizide and 23 percent less likely for empagliflozin.
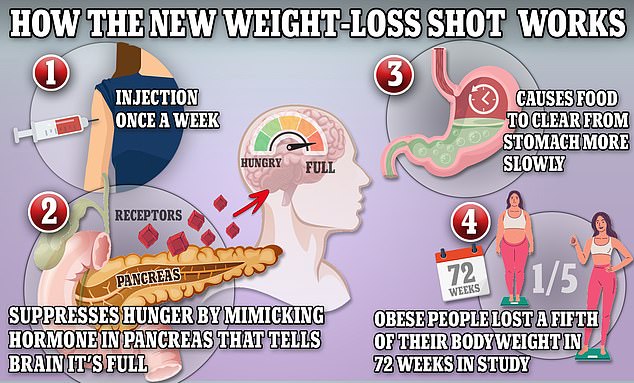
Weight loss drugs like Ozempic and Wegovy mimic the production of the hormone GLP-1, which helps keep the body feeling full.
The researchers, however, acknowledged that the study had “several limitations,” including not controlling for variables such as whether patients adhered to taking their medication regularly.
“As this study is observational, it cannot be proven that the observed outcomes are adverse drug events,” they added.
The injections have been shown to help users lose up to 33 pounds (15.3 kg) on average over 68 weeks.
They work by tricking the brain into thinking it is full, thereby reducing appetite and helping people lose weight as a result.
Semaglutide has been available on the NHS since 2019, and in the US since 2017, for type 2 diabetics. control blood sugar levels.
Another drug, semaglutide, was also approved in Britain for weight loss in 2022, and in the United States in 2021, under the brand name Wegovy.
Like any medicine, semaglutide can cause side effects that vary in frequency and severity. Reported problems include nausea, constipation, diarrhea, fatigue, stomach pain, headaches, and dizziness.
Strange symptoms, such as hair loss, have also been reported in some patients.
The latest figures from the National Health Service (NHS) show that 26% of adults in England are obese and a further 38% are overweight but not obese. In the United States, an estimated 41.9% of the adult population is obese.
Although hormone-mimicking injections are designed to help overweight patients become healthier, there has also been growing concern about the number of normal-weight and underweight patients taking them for cosmetic reasons.
Some have even needed emergency room care after receiving vaccines in an attempt to get a “beach-ready” body.


