Millions of Americans who take cholesterol-lowering pills may not need them and could be at risk of side effects such as liver damage.
Using a new risk calculator, researchers estimated that 40 percent of people in the U.S. who take statins to prevent heart disease will not actually develop the condition.
That number adds up to about 17 million Americans, including 4 million currently taking statins, who would no longer need to take the pills.
If the findings are translated into new recommendations and policies, they could have enormous consequences. As one of the most popular drugs in the United States, statins represent a $15 billion industry, which is expected to grow to $22 billion by 2032.
And for patients, the pills have been linked to a number of unpleasant side effects, including headaches, muscle aches, liver damage and problems with blood clotting.
Statins, taken by millions of Americans, are a cheap class of drugs aimed at lowering cholesterol, reducing the risk of heart disease and stroke.
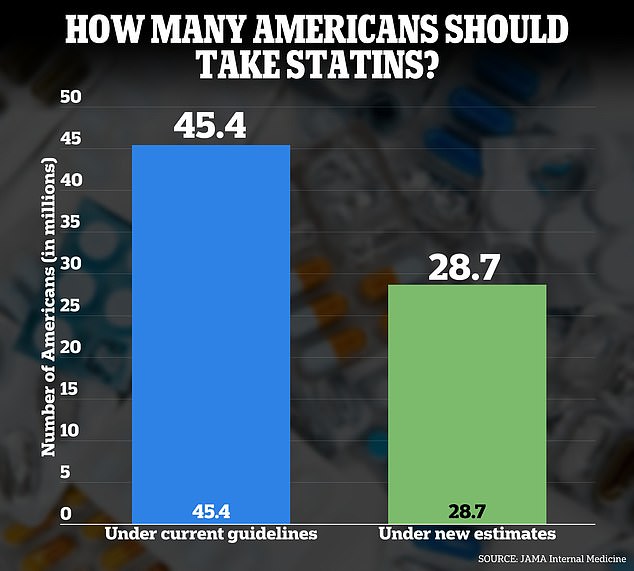
Researchers in a new study published in JAMA Internal Medicine found that fewer Americans need to take statins than previously thought, amounting to more than 17 million patients.
However, experts warn patients not to suddenly stop taking statins, as they can cause “dangerous” side effects such as heart attacks and strokes.
Dr. Chiadi Ndumele, chair of one of the American Heart Association’s (AHA) scientific advisory groups, said that while no new guidelines have been implemented, “analysis is underway.”
“Guidelines will need to consider whether and how to update recommendations to include PREVENT risk thresholds to guide clinical decision-making,” he said. Statistical news.
Statins work by limiting the production of “bad cholesterol” (low-density lipoprotein (LDL) cholesterol), which can harden and narrow the arteries and increase the risk of cardiovascular disease.
They are usually taken in the form of daily pills and cost as little as $40 a year for patients.
Because they are so cheap to produce, statins such as atorvastatin (Lipitor) have become some of the most popular medications in the United States.
Current guidelines from the AHA and the American College of Cardiology state that adults with at least a 7.5 percent 10-year risk of developing heart disease are recommended to take a statin.
At a five percent risk, guidelines suggest the patient and their doctor should consider it.
Your risk is based on factors such as BMI, cholesterol, smoking, and diabetes.
But in November, the AHA unveiled a new risk calculator called PREVENT, which estimates a patient’s 10- and 30-year risk of developing heart disease based on the health of the heart, kidneys and metabolism.
PREVENT (Prediction of Risk of Cardiovascular Disease Events) is a calculator used to assess the risk of heart disease, stroke, kidney disease, and heart failure.
Ask patients their sex, age, and risk factors such as cholesterol, blood pressure, BMI, diabetes, and smoking.

The CDC estimates that statins reduce the risk of heart attack by 25 percent, although the drug has been linked to side effects such as headaches, diarrhea and liver damage.
In the new research, published Monday in JAMA Internal MedicineThe team analyzed data from 3,785 adults ages 40 to 75 who participated in the CDC’s National Health and Nutrition Examination Survey between January 2017 and March 2020.
The researchers estimated participants’ 10-year heart disease risk using a 2023 PREVENT model and then compared the risk estimates to the 2013 Pooled Cohort Equations (PCE), on which current statin guidelines are based.
They found that 28.3 million Americans are eligible to receive statins, compared to 45.4 million under current guidelines.
Meanwhile, the UK’s National Institute for Health and Care Excellence (NICE) agency, which sets healthcare guidelines, recommends that patients can receive statins if they have a risk score of less than 10 percent and They have not had a heart attack or stroke.
However, statins have long been mired in controversy due to a number of studies claiming they cause side effects.
In the United Kingdom, health officials warned against seven statins, including atorvastatin (Lipitor) and rosuvastatin (Crestor), which were linked to myasthenia gravis, a serious condition that weakens muscles.
While the disease does not affect the life expectancy of most people, it can be life-threatening if it weakens the muscles needed for breathing.
According to the Cleveland Clinic, the pills have also been linked to headaches, nausea, dizziness, gas, diarrhea, constipation, memory loss, and liver and kidney damage.
However, a team of cardiologists from the Medical University of Lodz (Poland) stated in 2022 that 70 percent of the side effects of statins are “all in the mind.”
They called this the “nocebo” phenomenon, which occurs when someone faces an uncomfortable side effect of a medication simply because they expected it.
Meanwhile, Dr. Leslie Cho, a cardiologist at the Cleveland Clinic, warned at a hospital blog entry that stopping taking statins without telling your doctor could cause your cholesterol to rise rapidly, resulting in an increased risk of heart attack, stroke, and heart failure.
“High cholesterol is a silent killer because you won’t feel anything until something extreme happens,” he said. ‘Keep taking your statins. Stay well.’


