Hundreds of Americans have joined a multistate lawsuit alleging that the creators of Ozempic and Mounjaro caused life-threatening stomach paralysis.
The lawsuit was filed against Novo Nordisk and Eli Lilly, pharmaceutical giants that have raked in billions from blockbuster diabetes and obesity drugs.
Dana Filmore, an Ohio native and grandmother of seven, can no longer eat solid foods and has to blend her meals. Jacqueline Barber of Louisville vomited so much that she became dangerously malnourished.
Bob Tuttle, an oil rig worker in Tennessee, was forced to quit his job because his stomach pain was unbearable. And Philadelphia-born Debbie Kirtz believed she would never leave the hospital alive.
They and many others argue in the lawsuit that Lilly and Novo failed to warn their millions of enthusiastic customers about the very real risk of serious gastrointestinal injuries, including stomach paralysis, gallbladder problems, colon removal and more, in addition to making misleading statements about drug safety.
Dana Filmore of Columbus, Ohio, now subsists on a diet of protein shakes and gelatin. His stomach paralysis linked to Ozempic prevents him from eating solid foods
Dana Filmore, a 55-year-old diabetic, was uncomfortable with the prospect of having to stick herself with a needle every week when her doctor suggested she try Ozempic to manage her type 2 diabetes.
For about two years, the drug did what it was approved for: lowered her blood sugar levels. But in the last six months that she was taking this, she developed severe nausea. He gradually worsened and had to spend his vacation recovering.
It got to the point where she was afraid to eat solid food, because just a few bites would send her to the bathroom.
she said USA today: ‘Solids are really difficult for me. My body just rejects it.’
He was recently diagnosed with gastroparesis, or stomach paralysis.
It causes the contractions of the stomach muscles to become too weak to digest food and pass it to the intestines, causing food to stay in the stomach longer than it should.
When the stomach releases food, instead of gradually and steadily, it is emptied in larger, unprocessed bursts, causing chaotic diarrhea.
Mrs Filmore, who had to excuse herself just minutes after starting to eat, said: “You never know what might trigger it.”
He has even interrupted his 35-minute commute to work, where he manages a team of technicians at a mechanical company.
She said: ‘Halfway to work, I have to stop at a restaurant or a gas station. My stomach doesn’t give me much time to really decide where I’m going to go.’
His diet now consists mainly of protein shakes and gelatin. It’s the only meal plan that prevents you from running to the bathroom.
In Louisville, Kentucky, Jacqueline Barber, another plaintiff in the case, was also diagnosed with life-threatening gastroparesis.
He was prescribed Ozempic for his type 2 diabetes in 2021, but spent every night for more than a year sleeping on the couch next to a trash can to control his uncontrollable vomiting.
The 48 year old man saying: “Lying on the couch and vomiting non-stop, barely being able to walk, going anywhere, it’s very depressing.”
The only thing he could keep down were peanuts, peanut butter cookies, and peanut butter cookies.
‘I ended up losing 140 pounds. I weighed about 87 pounds, couldn’t walk or move, couldn’t get off the couch. Nobody knew what was happening. Nobody put the two together.


Jacqueline Barber of Louisville, Kentucky was diagnosed with stomach paralysis after taking Ozempic to control her diabetes.
Mrs Barber had to be connected to a feeding tube.
“My stomach was paralyzed,” he said. “I couldn’t tolerate anything.”
Meanwhile, Bob Tuttle, 60, a Tennessee native, was 60 miles offshore on an oil rig in the Gulf of Mexico when had to be transported by plane by helicopter to the emergency room after four days without being able to keep food down.
He was diagnosed with stomach paralysis within a week related to the Ozempic he had been prescribed in 2018.
Mr Tuttle, a safety and environmental advisor on the platform, was healthy and fit, a necessity for the job, which includes lots of stairs and running.
The medication successfully controlled his A1C levels and kept his diabetes under control. But little by little he began to lose weight without trying. He became increasingly fatigued and, later, severely nauseous.
He received his diagnosis just days after leaving the oil rig: ‘Gastroparesis, in simple terms, is simply the inability of the stomach to process solids or liquids that one ingests.
“My stomach was processing some of the liquids, but none of the solids during the tests they did on me at the hospital.”
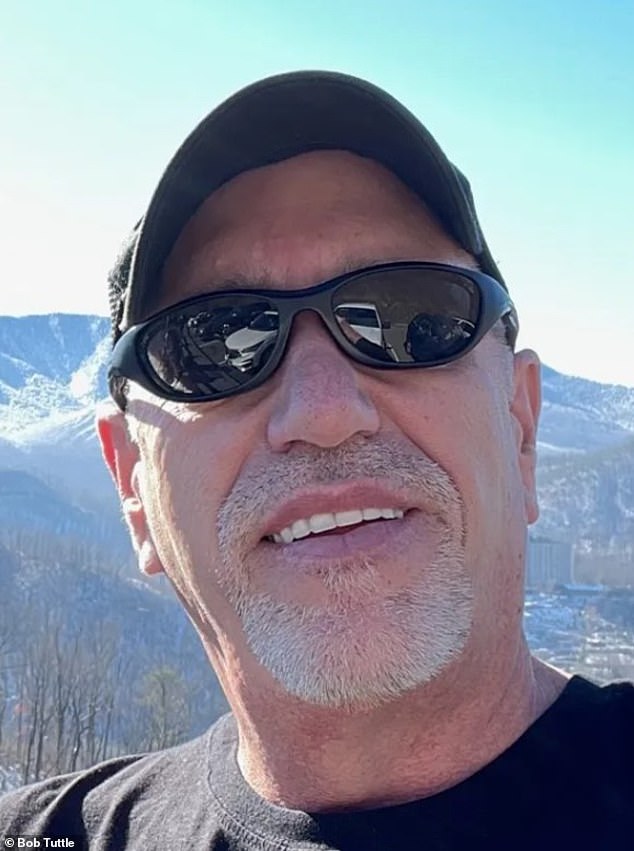
Bob Tuttle of Tennessee became so sick from his stomach paralysis that he had to quit his job as a safety advisor on an oil rig.

Tuttle had to be airlifted from the platform in the Gulf of Mexico after four days of being unable to keep food down. He was diagnosed with stomach paralysis a week later.
Now off drugs and no longer chronically nauseous, Tuttle still had to quit her job to deal with the illness.
Tuttle has joined the lawsuit against the companies.
Novo and Lilly have denied accusations that their drugs cause stomach paralysis.
A spokesperson for Novo Nordisk said there is no basis and that the risks of semaglutide, the active ingredient in Ozempic, are clearly stated on the label.
They added: “Novo Nordisk stands behind the safety and effectiveness of all of our GLP-1 medications when used as directed and when taken under the care of a licensed healthcare professional.”
Ozempic FDA Approved warning label mentions “gastrointestinal adverse reactions” and none of those listed include gastroparesis.
Nearly 22,000 adverse reactions to Ozempic have been recorded in the FDA’s Voluntary Adverse Event Reporting System. Gastrointestinal conditions, such as stomach paralysis, account for 43 percent of those reports.
That doesn’t mean the 22,000 injuries were actually caused by drugs. And considering that millions of people take these drugs every day, doctors say the injections’ panel of side effects is pretty safe.
Now that a few years have passed since the introduction of Ozempic for people with diabetes, researchers can better track the long-term effects of taking the drug beyond helping people lose some weight.
Researchers at the University of British Columbia studied a swath of medical records between 2006 and 2020 from people who took liraglutide, another diabetes drug semaglutide, and another drug called bupropion-naltrexone.
the researchers found that people who use semaglutide for weight loss, which works by binding to GLP-1 receptors in the pancreas and brain to reduce appetite and control cravings, were 9.1 times more likely to develop pancreatitis (inflammation of the pancreas) , a condition that can sometimes require surgery.
Additionally, semaglutide users were 4.22 times more likely to experience intestinal obstruction, a life-threatening condition, and had a 3.67 times greater risk of developing gastroparesis (often called “stomach paralysis”), which slows or stops the movement of food from the stomach to the small intestine.
In a trio of studies To analyze the effects of GLP-1 agonists, a class that includes Ozempic and Wegovy, on gastrointestinal health, researchers examined real-world data from patients who were prescribed one of the drugs between 2021 and 2022. They compared it to a control group of diabetics or obese people who were not prescribed the medications.
Patients taking GLP-1 were 66 percent more likely to be diagnosed with gastroparesis compared to those not taking the drug.


