Mask mandates appear to be quietly returning to hospitals across the United States amid growing concerns about what experts call a “quadremic.”
Four viral infections (flu, Covid, the cold-like virus RSV and norovirus) are on the rise, reaching around 15 million cases and 30,000 deaths so far this winter.
In response to the outbreak, Duke Health in North Carolina and Mass General Brigham in Massachusetts updated their mask-wearing and visitor guidelines this week.
It means hospitals in at least eight states are requiring or strongly urging the use of masks indoors, including Wisconsin, California, Illinois, Indiana, New Jersey and New York.
The move comes amid growing fears about a viral outbreak in China that has reportedly overwhelmed hospitals in northern provinces.
Mass General, which treats 2.5 million patients, is made up of 12 hospitals and clinics spread across Massachusetts, and at most of its facilities, leaders raised their respiratory virus activity status to “high.”
Doctors and hospital staff are now required to wear masks in patient areas and patients and visitors are “strongly encouraged” to wear a face mask, although there is no requirement.
In North Carolina, Duke Health hospitals and clinics stated: “Due to the increase in respiratory illnesses in our communities, we are updating our visitation restrictions after consulting with our infectious disease and infection prevention experts.”
The Mass General Brigham system in Massachusetts updated its visitor and masking guidelines this week

With dozens of locations across the state and surrounding areas, Duke Health now “strongly” recommends the use of masks in patient areas, and mask use is required in “select patient care areas based on medical condition.”
Additionally, visitor guidelines have been updated on a unit-by-unit basis, with some restrictions in place and a requirement for full personal protective equipment for the most vulnerable patients.
Elsewhere in the country, a spokesperson for Wisconsin’s Aurora Health Care system (which treats 1.2 million patients annually) confirmed According to local media WISN12, starting next week, masks will be required for patients and others in “congregated areas, such as patient rooms.”
New Jersey’s largest hospital system, RWJBarnabas Health, which cares for 3 million patients annually, has also reinstated its mask mandate.
In guidance posted online, the hospital system said that “all visitors are expected to wear a face mask and “maintain physical distancing.”
He added: “We will offer you a new mask for source control or we may ask you to replace your own mask with a hospital supplied mask.”
In San Francisco, anyone working in skilled nursing facilities must wear a mask. In Alameda, San Mateo, Contra Costa and Napa counties, as well as the city of Berkeley, healthcare workers and staff at certain care facilities are required to wear masks in patient areas.
In San Mateo, the mandate also applies to visitors.
In Illinois, the OSF HealthCare network, which has 10 locations in the state, requires all employees, patients and visitors to wear masks and temporarily restricts visiting hours and subsidies.
Data until December 28
Additionally, Rush University Health System, which includes two medical centers and a hospital, also began requiring face masks for staff and visitors.
In Indiana, Union Health also asked people to wear face masks and restricted visiting hours, citing rising flu, Covid and RSV cases.
Patients experiencing respiratory symptoms “are required to wear a mask when presenting to any Union Health facility,” which includes about three dozen locations across Indiana.
In New York, State Health Commissioner Dr. James McDonald declared last month that influenza is prevalent throughout the state and required health care workers who have not received this year’s flu vaccine to use masks in certain healthcare settings.
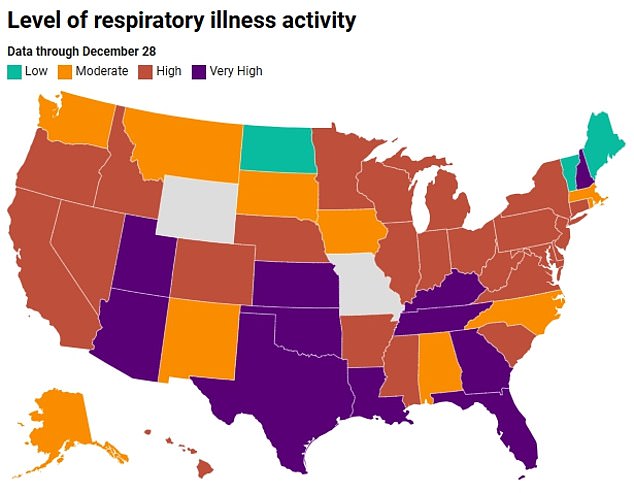
According to the CDC, the level of respiratory disease activity in the U.S. is “high” and is “high” or “very high” in most states.
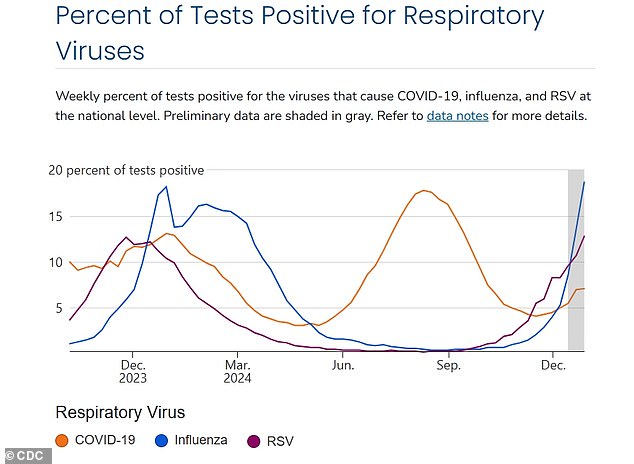
The virus with the highest level is Covid-19. Flu and RSV are at “moderate levels.”
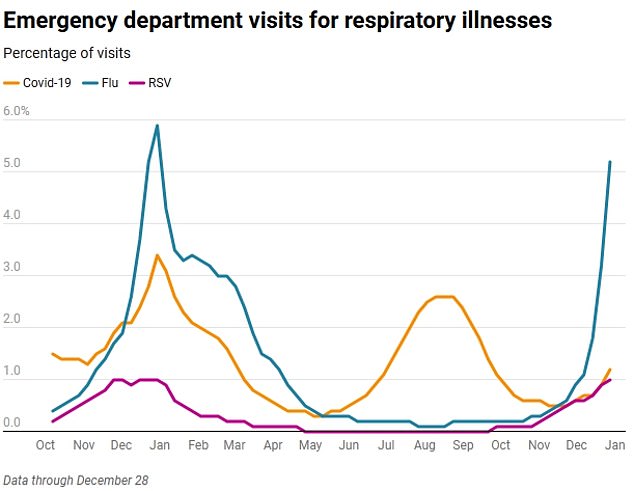
However, emergency room visits for flu and RSV are “very high” and increasing, while visits are “low” but increasing for Covid-19.
Flu and RSV cases reached new highs this season, with 19 percent and 13 percent of samples testing positive for those viruses in the week ending December 28.
About seven percent of tests came back positive for Covid.
The CDC estimates that there have been 1.2 million RSV visits, 60,000 hospitalizations and 3,100 deaths between October 1, 2024 and December 14.
For Covid, the estimates are 4.9 million cases, 1.1 million visits, 130,000 hospitalizations and 15,000 deaths.
And in the case of the flu, estimates are 9.3 million cases, 4.2 million visits, 140,000 hospitalizations and 13,000 deaths in the same period.
For the week ending December 28, the latest available, 1.2 per cent of hospital visits were for Covid, up from less than one per cent the previous month.
RSV accounted for one percent, up from 0.6 percent the previous month, and flu visits accounted for 5.2 percent of visits, a sharp increase from just one percent in the week that ended on November 30.
Hospitalizations have also increased for all respiratory viruses. Hospitalization rates increased to two percent for Covid and RSV and four percent for flu in late December.
Deaths increased slightly, but accounted for less than one percent of overall death rates.
Data shows that cases of norovirus, also called stomach flu, are at their highest level for this time of year since 2012.
State health departments reported 91 norovirus outbreaks (considered a cluster of two or more cases stemming from a common source) during the week of Dec. 5, up from 69 the week before.
In 2021, there were only two outbreaks during the same week.
Current data is not complete and the number of cases is likely higher than reported. The CDC does not report individual cases because the infection usually resolves on its own within a few days and is not diagnosed by a doctor or reported.
Just over a dozen states participate in the CDC’s national disease surveillance system.
Overall, norovirus is estimated to infect about 21 million Americans each year, sending about 2 million of them to doctors’ offices or urgent care. Approximately 465,000 people with the virus go to the emergency department each year and 900 people die.


