NHS hospitals are reinstating pandemic-like measures, such as mask requirements and visitor restrictions, in a bid to curb the spread of the epidemic.
Healthcare providers across the country are said to be buckling under the pressure of four winter viruses attacking the public at the same time: flu, Covid, norovirus and respiratory syncytial virus (RSV).
The flu is the main virus of concern, and hospital cases have multiplied by six in some areas.
Nationally, flu-related hospitalizations are three and a half times higher than this time last year, according to the most recent data.
Some experts are now worried about a new threat to NHS capacity, amid reports of rising cases of another respiratory virus, called human metapneumovirus (HMPV), which is said to be behind a worrying outbreak in China.
An example of the strict new measures comes from the Royal Bolton Hospital, where all staff, patients and visitors are now required to wear a mask on site.
Other mask mandates have been introduced by Liverpool University Hospitals NHS Foundation Trust and University Hospitals Birmingham NHS Foundation Trust.
Meanwhile, Shrewsbury and Telford Hospital NHS Trust, Mid and South Essex NHS Foundation Trust, Cambridge University Hospitals NHS Foundation Trust and Worcestershire Acute Hospitals NHS Trust are now restricting visitors from seeing patients.
It comes as several NHS hospitals, including Liverpool University Hospital, have declared critical incidents due to increasing demand in A&E, including mammoth 50-hour waits in some emergency departments.
NHS hospitals are reinstating Covid pandemic measures such as mask requirements and visitor restrictions in a bid to curb the spread of the pandemic. Pictured by staff at King’s College Hospital in 2021

The Royal Bolton Hospital is among those asking all staff, patients and visitors to wear masks to combat the rise of winter pathogens such as flu.
This means trusts can no longer ensure that critical care can be provided.
Declaring such an incident can allow hospitals to take steps such as canceling non-urgent operations and asking furloughed staff to return to work to help meet emergency demand.
Speaking about the mask mandate, Tyrone Roberts, head of nursing at Royal Bolton Hospital, said: “We are seeing a large number of flu cases in our hospital, and it is important that we take action to address this to protect our patients, staff and visitors, since for some people the flu can be a very serious illness.
“We are asking for your help to stop the spread of the flu and other winter illnesses by wearing a mask when entering patient areas of our hospital, such as wards.”
He added that the Trust expected mask-wearing measures to continue until flu cases peaked in the coming weeks.
Meanwhile, Oliver Zuzan, medical director at Royal Liverpool University Hospital, said of its “critical incident”: “We have taken this action to support the safe care and treatment of our patients, which is our absolute priority.”

Patients in Royal Liverpool University Hospital’s emergency department are facing mammoth 50-hour waits, hospital bosses have warned as it faces a wave of people hit by respiratory illnesses such as flu.
“Colleagues are working incredibly hard to treat people as quickly as possible, however some people will experience longer waits as we treat our sickest patients.”
This was joined by several trusts across the country, with NHS Cornwall and Isles of Scilly also declaring a critical incident on Friday last week.
Margaret Garbett, head of nursing at University Hospitals Birmingham NHS Foundation Trust, said: ‘This significant and sustained pressure is due in part to the exceptional number of flu patients requiring hospital admission; There are now 311 patients in hospital and measures including the use of masks are also being introduced in all departments.’
In a new statement, NHS national medical director Professor Sir Stephen Powis said demand in hospitals “shows no signs of abating”.
“The latest data shows flu cases soared to around 5,000 a day in hospitals at the end of last year and multiple trusts across the country declared incidents to help them manage the additional pressure on services,” he said.
“In addition to flu, hospitals are also experiencing continued pressure from Covid, RSV and norovirus cases, as the “quadraemia” continues to increase pressure on all services.”
‘Anyone who needs medical support should continue to use services as normal – the NHS website, NHS 111 and 111 online are available if you need advice and support for health issues, community services such as GPs and pharmacies are open as always for help and advice. while you can use 999 or attend A&E in life-threatening emergencies.’
Shrewsbury and Telford Hospital said it had made the “difficult” decision to reduce hospital visits due to rising numbers of flu, Covid and other winter illnesses.
She added that exemptions apply, such as when a patient is dying, receives a life-limiting diagnosis, needs support to communicate or is a child, and for birthing partners.
Paula Gardner, acting chief nursing officer at Shrewsbury and Telford Hospital NHS Trust, said: “This will protect our most vulnerable patients and reduce the growing spread of infections.” We also ask all patients, visitors and staff to wear masks and practice good hand hygiene.
At Broomfield Hospital in Chelmsford, visitors are not allowed in the emergency department, acute medical unit, except for patients receiving end-of-life care, the trust added.
Cambridge University Hospitals NHS Foundation Trust has implemented additional visiting restrictions due to the increasing number of norovirus, flu, RSV and Covid cases in hospitals.
Experts have warned that hMPV, which produces flu-like symptoms, can remain in the body for days and can therefore easily be transmitted to other people.
For all adult inpatient areas, visiting hours have been reduced from 3:00 pm to 6:00 pm; For all areas, including wards and the emergency department, a maximum of one visitor is permitted at a time, who must be over 12 years of age. There are also restrictions for pediatrics.
Additional visits may be allowed on compassionate grounds, and the trust added that this should be discussed and coordinated with the ward.
All visitors will be required to wear a mask in clinical areas.
Worcestershire Acute Hospitals NHS Trust said it will only allow patients to be accompanied by one person in all areas of the emergency department to prevent further spread of flu.
It added that it may restrict visits due to flu, Covid and RSV outbreaks, and advised people to check with the ward before visiting.
Despite mounting pressures, the latest official data shows that just under one in four frontline healthcare workers in England have had the flu vaccine this year.
It comes amid concerns that another winter virus, hMPV, could also place additional pressure on NHS services in the coming weeks.
Official data shows One in 10 children tested for respiratory infections in the hospital tested positive for hMPV as of December 23.
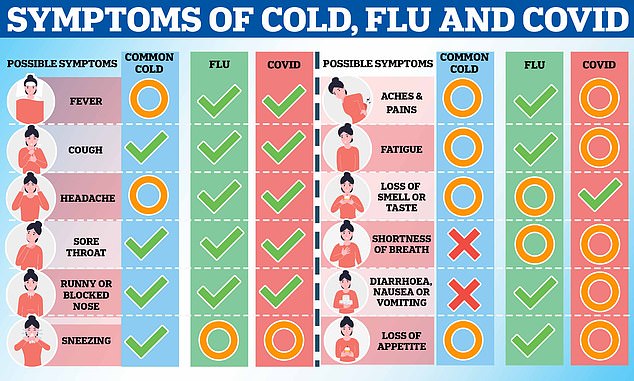
The graph shows common symptoms (green checkmark), occasional and possible symptoms (orange circle) and symptoms that never occur (red cross) with the common cold, flu and Covid.
This is more than double the proportion of very young children who tested positive for hMPV at the end of November.
While hMPV primarily causes mild illness similar to the common cold, very young children, along with the elderly and those with weakened immune systems such as cancer patients, are at increased risk of severe illness.
Concerns emerged after distressing images of Chinese hospitals inundated with hMPV patients.
However, UK officials say levels in Britain are currently what would be expected for this time of year.
The latest NHS data, covering the week to December 29, shows that flu patients occupied around 4,500 beds every day last week, 3.5 times more than in the same week last year.
Of those, 211 were in critical care, 69 percent more than the previous week.
More than 4,100 Britons also spent Christmas Day in hospital with flu. By December 29, this number had increased to more than 5,000.
Meanwhile, rates of norovirus, the winter vomiting bug, are also 40 percent higher than expected for this time of year.
Experts have warned that the situation could get worse before it gets better as Britons fall ill from the cold weather and from infections with viruses acquired through socializing over the festive period, increasing potential pressure on NHS services.


