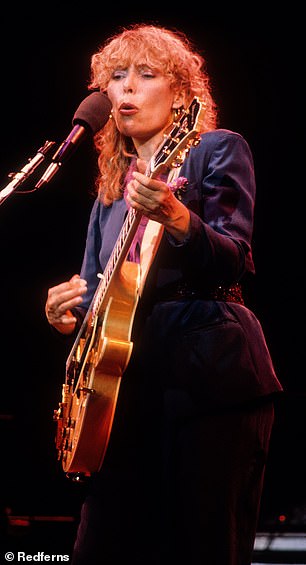
Music legend Joni Mitchell, 80, made her Grammy debut at the awards show on Sunday and took home a gold trophy for Best Folk Album.
The album, recorded in 2022, was a surprise performance by the musician who had stepped away from the spotlight in 2015 after suffering a brain aneurysm.
But Mrs. Mitchell, 80, also revealed that he suffers from a “strange and incurable” disease called Morgellons disease.
Cause ‘Fibers in a variety of colors stick out from my skin like mushrooms after a storm,” he told the Los Angeles Times in 2010.
However, despite similar patient reports, the syndrome is not recognized by major US health agencies and medical professionals often refer to it as a “delusional” illness.
Joni Mitchell revealed in a 2017 biography that she suffers from a mysterious illness called Morgellons disease.

Mitchell made her Grammy debut at the awards show on Sunday, taking home a gold trophy for Best Folk Album.

Ms. Mitchell said in 2010 that the disease causes “various colored fibers to stick out of my skin like mushrooms after a storm.”
The condition has no known organic basis and is believed to be a psychiatric condition.
The disease, according to the Mayo Clinic, is characterized by the belief that parasites or fibers are embedded under and protruding from a person’s skin.
People with Morgellons report feeling like something is crawling on their skin or itching and describe severe itching and sores.
Some healthcare providers classify the condition as a delusional infestation and prescribe antidepressants and antipsychotics to treat it, along with therapy and counseling.
Other providers attribute the symptoms to skin cell infections.
The medical community at large says more research needs to be done on MS.
Symptoms of MS include very itchy skin rashes and sores, tingling sensations on or under the skin, the belief that there are fibers, threads or threads under the skin, muscle and joint pain, depression and inability to concentrate.
More than 14,000 people are estimated to be affected by the disease, according to Medical News Today.
TO study in 2018 in the journal Clinical, Cosmetic and Investigational Dermatology, said the skin condition is characterized by the presence of multicolored filaments and fibers that are embedded in or projecting from the skin.

The enlarged photo above shows blue and white filaments embedded in the skin from a 2018 study.

The enlarged photo above shows blue filaments embedded in the skin from a 2018 study.
A disease with these characteristics was reported for the first time in the United States in 2002.
The study authors wrote: “Because individuals affected by the illness may have tingling or stinging sensations and sometimes believe they have an insect or parasite infestation, most doctors consider MS a purely delusional disorder. “.
Research on this condition has yielded mixed conclusions.
The 2018 study said some research ignores the fact that some mental health disorders may be the result of an underlying illness.
Additionally, other experimental research has shown that the skin condition could be a physiological response to an underlying infection.
In 2012, the Centers for Disease Control and Prevention study 115 people with Morgellons, what the agency calls “an explained dermatopathy.”
The study showed that most of the skin fibers and filaments could be explained by patients repeatedly scratching skin sores and fabric fibers entering those sores, as opposed to fibers emerging from the skin.
The researchers also noted that the condition is most frequently reported by middle-aged white women and that the symptoms are very similar to the condition delusional infestation.
It is a mental health disorder in which patients have false beliefs about being infested with parasites.
The study also estimated a prevalence of 3.65 cases of DM per 100,000 people in the United States.
No known cause of MD has been determined, but a 2015 study study explored the link between the skin disorder and Lyme disease and found that 24 of 25 DM patients had the tick-borne disease.
A case from 2021 report described a 27-year-old white woman with a history of anxiety, bipolar disorder, and depression who was experiencing MS-related symptoms.
The woman went to the emergency room with sores and skin ulcers after spending time in a heavily wooded area.


The photo on the left shows a hand injury on a patient and the photo on the right shows a thigh injury on a patient from a 2021 case study.

The above shows skin scrapings that revealed fibers and debris collected from various lesions on the patient from a 2021 case study.
Doctors believed he was suffering an allergic reaction and prescribed Benadryl and a steroid cream.
However, three days later she visited her primary care doctor complaining of a rash and saying that “worms were coming out of my body.” She also reported that she had seen a black insect that had “popped out” of one of her injuries.
He later identified the insect as a tick.
After several months of treatment, he continued to report that multicolored threads were emerging from his sores that caused stinging and burning.
She was referred to a dermatologist and given a two-week course of a powerful antibiotic, which led to significant improvement in the sores on her skin.
This has led providers to believe that antibiotics could be an effective treatment option for patients with suspected Morgellons.
However, because the disease is so poorly understood, there is no cure for it.

