Olivia Munn has revealed she was diagnosed with breast cancer last year – after undergoing four operations in the last 10 months.
The actress, 43, took to Instagram earlier today to post a surprise health update.
She wrote: ‘IIn February 2023, in an effort to be more proactive about my health, I took a genetic test that checks you for 90 cancer genes. I tested negative for all, including BRCA (the most known breast cancer gene).
‘My sister Sara had also just tested negative. We called each other and high-fived over the phone. That same winter I also had a negative mammogram.
‘Two months later I was diagnosed with breast cancer.’

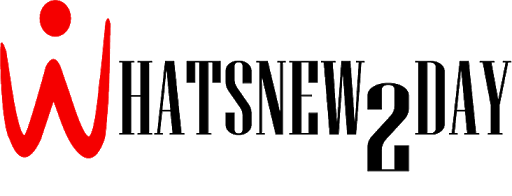
Olivia Munn has revealed she was diagnosed with breast cancer last year – after undergoing four operations in the past 10 months


The 43-year-old actress, who attended the 2023 Academy Awards this weekend, took to Instagram earlier today to post a surprising health update


She explained: ‘In the last ten months I’ve had four operations, so many days spent in bed I can’t even count’


Olivia, who attended the 2024 Oscars at the weekend with John Mulaney (pictured), thanked him for ‘the nights he spent researching what every operation and medication meant’
She continued: ‘In the last ten months I have had four surgeries, so many days in bed I can’t even count and have learned more about cancer, cancer treatment and hormones than I could have ever imagined.
‘Surprisingly I’ve only cried twice. I guess I didn’t feel like there was time to cry. My focus narrowed and I presented my emotions that I felt would interfere with my ability to remain clear-headed.
‘I’ve tended to let people see me when I have energy, when I can get dressed and get out of the house, when I can take my little boy to the park. I’ve kept the diagnosis and the worry and the recovery and the pain meds and the paper dresses private.
‘I needed to breathe and get through some of the hardest parts before I shared.’
Olivia went on to praise her OBGYN for decided to calculate her risk assessment score for breast cancer, adding: ‘The fact that she did saved my life.’
‘Dr. Aliabadi looked at factors like my age, family history of breast cancer and the fact that I had my first child after age 30. She discovered that my lifetime risk was 37 percent.
‘Because of that score I was sent to get an MRI which led to an ultrasound which then led to a biopsy. The biopsy showed that I had Luminal B cancer in both breasts. Luminal B is an aggressive, fast-moving cancer.
’30 days after that biopsy I had a double mastectomy. I went from feeling perfectly fine one day, to waking up in a hospital bed after a 10-hour operation the next.’
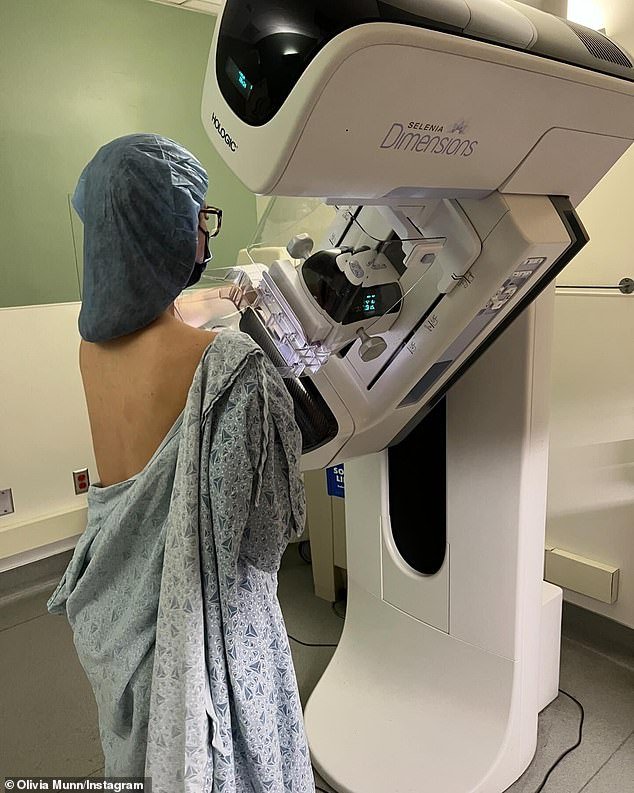
Olivia praised her OBGYN for deciding to calculate her breast cancer risk assessment score, adding: ‘The fact that she did saved my life’


Olivia revealed she had also undergone a double mastectomy, adding: ‘I went from being perfectly fine one day to waking up in a hospital bed after a 10-hour operation the next.’


Olivia, who is mum to two-year-old son Malcolm Hiep (pictured), wrote in her caption: ‘I hope that by sharing this it will help others find comfort, inspiration and support on their own journey’
John, 41, showed his support in a comment which read: ‘Thank you for fighting so hard to be here for us. Malc and I adore you.’
Olivia, who attended the 2024 Oscars at the weekend with John Mulaney, added: ‘I’m lucky. We caught it with enough time for me to have options. I wish the same for any woman who might have to face this one day.’
She then encouraged her followers to ask their doctors to calculate their breast cancer risk assessment scores as well as to insist that women keep up with their annual mammography and breast MRI.
‘I am so grateful to my friends and family for loving me through this. I am so grateful to John for the nights he spent researching what each surgery and medication meant and what side effects and recovery I could expect.
“For being there before I went to every operation and for being there when I woke up and always placing framed pictures of our baby boy Malcolm so it would be the first thing I saw when I opened my eyes, ” wrote the star.
Olivia concluded: ‘Thank you to the friends who have had breast cancer and the friends who connected me with friends who have had breast cancer for guiding me through some of my most uncertain and overwhelming months.
‘I am extremely grateful to the nurses, patient coordinators and staff at Cedars-Sinai in LA and Saint John’s in Santa Monica. I would like to specifically thank my surgical oncologist Dr. Armando Giuliano, my reconstructive surgeon, Dr. Jay Orringer, my oncologist Dr. Monica Mita and especially my guardian angel, Dr. Thais Aliabadi.’
Olivia, who is mum to two-year-old son Malcolm Hiep, wrote in her caption: ‘I hope by sharing this it will help others find comfort, inspiration and support on their own journey.’
John, 41, showed his support in a comment which read: ‘Thank you for fighting so hard to be here for us. Malc and I adore you.’