A Colorado woman was diagnosed with colorectal cancer after she thought her smelly gas was due to probiotics.
Jelena Tompkins was just 34 years old in 2016 when she noticed her gas smelled worse than before.
The mother of one had just run a half marathon and was maintaining a healthy diet, although she thought it might be due to something she was eating.
Tompkins started taking probiotics to balance her gut bacteria, but the smell didn’t improve. Shortly after, he noticed blood in her stool.
Jelena Tompkins was just 34 years old in 2016 when she noticed that her gas smelled stronger than usual. She was diagnosed with stage three rectal cancer.


Ms Tompkins had just run a half marathon before her diagnosis and was eating a healthy diet. “She was in the best shape of my life,” she told The Patient Story. ‘I ate healthy and never thought cancer would attack me at such a young age’
She attributed the symptoms to the probiotics, and at her annual physical a few months later, her doctor said the bleeding was simply due to dietary changes.
However, three months later, when Tompkins was not taking probiotics, doctors performed allergy tests to see if food intolerances had altered her digestive system.
Eventually, he underwent a colonoscopy, which revealed stage three rectal cancer that had spread to his lymph nodes.
“I was in the best shape of my life,” Ms. Tompkins said. The patient’s history. “I ate healthy and never thought cancer would attack me at such a young age.”
Colorectal cancer rates are rising around the world, causing an epidemic among young people.
Rates are expected to double among young people by 2030, and colorectal cancer is also expected to become the leading cause of cancer death in people under 50 by the end of the decade.
Colon and rectal cancers are the third most common type in the U.S. and the third leading cause of death in both men and women.
The American Cancer Society (ACS) estimates that about 153,000 cases of colorectal cancer will be detected in 2023, including 19,500 among those under 50 years of age.
About 53,000 people are expected to die from the disease this year.
Experts are still working to unravel the cause of this devastating epidemic. This change has commonly been blamed on unhealthy diets, alcohol consumption, and sedentary lifestyles.
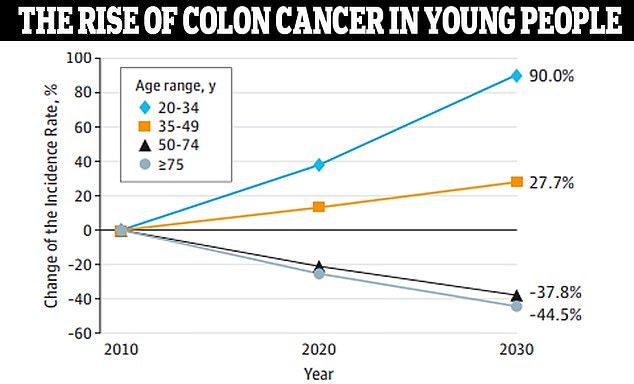
Data from JAMA Surgery showed that colon cancer is expected to increase by 90 percent in people ages 20 to 34 by 2030. Doctors aren’t sure what is driving this mysterious increase.

Ms. Tompkins underwent radiation and chemotherapy, with breaks to attend her sister’s wedding and participate in a local race.


Ms. Tompkins had 12 inches of colon and rectum removed, as well as 17 lymph nodes, and an ileostomy bag was placed.
Mrs Tompkins underwent 28 days of radiation and the chemotherapy pill Xeloda, also known as capecitabine, which is designed for late-stage colorectal cancer.
After another two months of rest, his tumor began to shrink, although he still needed surgery.
Doctors removed 30 centimeters of colon and rectum, as well as 17 lymph nodes, leaving five cancerous nodes.
Ms. Tompkins had an ileostomy, which is when surgeons make an opening in the abdomen and bring a piece of the ileum, the lowest part of the small intestine, outside the abdominal wall to create a stoma.
Digested food then passes through the stoma into an external pouch instead of passing through the rectum and anus.
Six weeks after surgery, he started FOLFOX combination chemotherapy, which he finished in May 2017, just in time to run in a local race.
Mrs Tompkins is now in remission and receives maintenance chemotherapy, as well as scans once a year.
Part of what makes colorectal cancer difficult to diagnose are its symptoms, which can often be attributed to other conditions. However, some stand out more than others.
A study published last year in the Magazine of the National Cancer Institute found that the most reported symptoms were abdominal pain, blood in the stool, diarrhea, and iron deficiency anemia.
Additionally, in a 2020 survey conducted by Colorectal Cancer Alliance, 68 percent of participants said they experienced blood in their stool. The average age of the participants was 42 years.
The same survey also found that many patients with colorectal cancer symptoms were initially misdiagnosed or ruled out.
More than half of those surveyed said they had been misdiagnosed with conditions such as hemorrhoids, irritable bowel syndrome, anemia and mental health problems. And patients ages 19 to 39 were more likely to feel dismissed by their provider.
In one study, it took an average of 10 months for a single symptom to receive a colorectal cancer diagnosis. Those with at least three symptoms were diagnosed after five months on average.

Ms Tompkins is now in remission and receives maintenance chemotherapy, as well as scans every year to look for recurrence.
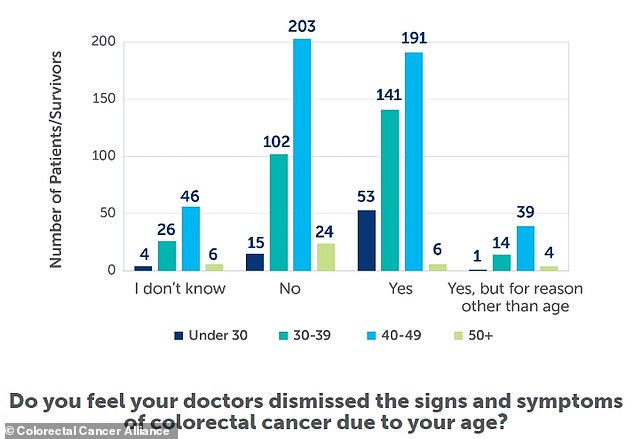
A 2020 survey from the Colorectal Cancer Alliance found that many patients with colorectal cancer symptoms were initially misdiagnosed or ruled out.
Standard colonoscopy begins at age 45, and Tompkins acknowledged she was lucky her doctor didn’t resist ordering one.
“If they refuse a colonoscopy, tell them that they must make a record in your file that you came to them with symptoms and that they refused to do a colonoscopy,” he said.
“That may also make them think twice before denying it.”
Since cancer is not hereditary, Ms. Tompkins sought support in online communities of other patients.
‘We could vent when we were really tired or ask, “Hey, is this bothering your system?” Or, “OMG, is your ileostomy going crazy too? What can you do to stop this? “What do you drink when you’re going through FOLFOX and you have that cold sensitivity and everything has to be hot,” she said.
“Those are some of the things you don’t necessarily bother your oncologist about, but having a supportive friend can help you exchange ideas and make you feel like you have a support group that’s there for you and who you can reach out to if you’re having a bad day.’


