Marit Peterson doesn’t remember much about her battle with cancer, but she has scars (physical and emotional) that serve as constant reminders.
When Texas was just a baby, his mother noticed a strange spot on the little boy’s finger.
After taking her daughter to several doctors, all of whom were ruled out, one finally agreed to remove it “for cosmetic reasons” in July 2006, when Marit was two years old.
But during surgery, doctors realized the severity of her condition. Tests revealed that Marit had stage 3 melanoma, the deadliest skin cancer in the United States.
In fact, Marit’s case was so rare that top oncologists at MD Anderson Cancer Center in Houston had never seen a melanoma patient so young before, and there were no survival statistics for patients her age.
Marit Peterson was diagnosed with melanoma at age two and underwent multiple surgeries on her right hand and arm to remove the cancer from her body.

Marit faced a year of high doses of immunotherapy drugs and the little girl had to have a port implanted in her chest to receive the medication.
For adults, it was six months.
But now, Marit, a 20-year-old pre-med student at the University of Texas at Austin, told DailyMail.com: “Having the perspective and perception that I’m not supposed to be here has made me who I am today, and it’s shaped my personality and what I want to do with the rest of my life.”
His message? Don’t wait any longer, go to the doctor and don’t take “no” for an answer.
Marit’s mother, Candy, first noticed a spot on her baby’s hand when he was three months old.
Her father had survived melanoma and Candy thought the little girl’s mole looked a lot like her own.
Although she had “suspicions,” Candy, who was diagnosed with cancer at age 34, did not take the baby to the doctor immediately.
Only about 500 children are diagnosed with pediatric melanoma each year in the U.S., so in his opinion, it was highly unlikely.
Instead, she kept a close eye on the spot, but it started to grow, and that’s when Candy took her daughter in to get it checked out.
Several doctors told her it was benign and they wouldn’t remove it until one finally relented. But Candy said she agreed only because “she wants her daughter to look pretty. I understand; it’s cosmetic,” Marit told DailyMail.com.
However, once in the operating room, surgeons discovered that the mole was more invasive than they thought and immediately sent him for a biopsy.
Candy’s mother was shocked by the diagnosis since her two-year-old daughter had barely been exposed to the sun.
But Dr Michelle Henry, a dermatologist and winner of the Melanoma Research Foundation (MRF) Excellence in Prevention Award for her melanoma advocacy, told DailyMail.com that while melanoma is primarily caused by the sun, genetics also play a role and people with a family history of the cancer are at higher risk.
She said: “If you have a family history, there’s a certain level of vigilance you’ll need to have even more than people who just follow the standard (sun protection) rules.”
Stage 3B melanoma meant the cancer had spread from Marit’s right hand to the lymph nodes in her right armpit, and she had to undergo multiple surgeries.
She then had to spend a year on high doses of immunotherapy drugs. The little girl had to have a port implanted in her chest to receive the medication for a month and then her mother had to give her injections three times a week for a year.
Marit told this website: “The treatment made me very sick, with a fever of 105 degrees and I was on the verge of having seizures. I started losing my hair. It was scary. At night I had night terrors.”
And although she has since been declared cancer-free, the scars on her body are a daily reminder of her battle.

Marit has been a strong advocate for melanoma prevention, awareness and research and will receive this year’s Courage Award at the Melanoma Research Foundation Gala in October.

Marit has traveled to Washington, DC to speak with legislators about melanoma funding and has worked with the FDA to seek approval for new sunscreen ingredients.
In addition, the surgery on her armpit left her with nerve damage, which causes her residual pain.
She is also concerned about her fertility, as doctors are unsure whether her treatment had any effect on her ability to get pregnant.
Marit told DailyMail.com: “I really want to be a mother. I love my mum. She’s my best friend and I want to be like that with my children.”
Since her pre-teens, Marit has spoken publicly about her experience and has even traveled to Capitol Hill to meet with lawmakers about funding for melanoma, the deadliest form of skin cancer that claims the lives of nearly 8,300 people each year, according to the MRF.
Her family has raised more than $3 million for melanoma research, which has led to the identification of genes that may pose a higher risk of developing the disease. These new genes have been dubbed the “Marit Peterson genes.”
Now, Marit’s journey and efforts have made her the recipient of the Courage Award at next month’s event. MRF Galaand is excited to continue her advocacy.

Dr. Michelle Henry said people with a family history of melanoma should be especially vigilant when it comes to sun care.
The American Cancer Society estimates that 200,300 people will be diagnosed with some form of melanoma by 2024.
The average lifetime risk of developing melanoma is three percent, or one in 33 people, but the risk increases if a person has a family history of the disease.
There are several types of melanoma: cutaneous melanoma, which appears on the skin and is the most common; ocular melanoma, which develops in the eyes; and mucosal melanoma, which can appear in the sinuses, nasal passages, mouth or vagina.
There are also pediatric, adolescent and young adult melanomas.
Rates of new melanomas vary: in people under age 50, they have remained stable among women and have declined by about one percent per year in men since the early 2000s.
The five-year survival rate for melanoma is 94 percent, but that rate drops to 35 percent for melanomas that have spread and could be even lower depending on how far the cancer has progressed.
Annual full-body skin checks are recommended to detect cancer early, but people can perform regular self-checks at home and visit a dermatologist if they feel anything suspicious.
“Trust yourself. I tell my patients, ‘You know your body best, and part of advocating for yourself is not taking no for an answer,'” Dr. Henry said.

Marit (fourth from left) is a pre-med student at the University of Texas at Austin and is in the Zeta Tau Alpha sorority.
When performing self-screening, people should keep in mind the ABCDE principles of skin cancer.
A is for asymmetry: Is the mole symmetrical on all sides? Melanomas are often uneven, with halves of different sizes and shapes.
B is for border: Does the mole have clear borders? Melanomas are more likely to have jagged or irregular borders.
C is for color: Is the color the same throughout the mole? Melanomas are more likely to have multiple shades.
D is for diameter: How big is the mole? They should usually be about the size of a pencil tip, and melanomas tend to be larger.
Finally, E is for evolution: has the mole changed over time? Most benign moles stay the same from year to year, but melanomas can grow in size and shape and change color over time.
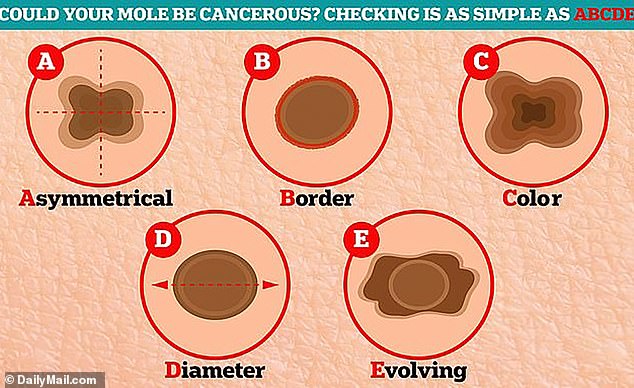
Annual full-body skin checks are recommended, but people can perform regular checks at home. When performing the exam, people should be aware of the basics of skin cancer.
Dr. Henry is excited about new detection and treatment tools that go beyond a simple skin check, including a new medical tape that noninvasively takes specks from a suspicious mole and sends them to be genetically analyzed to assess melanoma risk.
She said she sees many patients who are “so anxious” about developing melanoma that “it keeps them up at night and they can’t concentrate.”
But he is hopeful about the future of prevention and treatment: “We are getting better and better at refining our diagnosis and establishing risk.”
“And then we’re getting better and better at prevention: finding[moles]earlier, seeing them earlier, and looking at genetic data to get insights into how that mole might behave.”
As for Marit, she still faces the anxiety of having to go to MD Anderson Cancer Center every year, but she hopes to graduate from college, complete medical school and study dermatology, where she can help patients like her.
She said: ‘Some days I wake up and I’m scared I have cancer again and because I have to go back every year, (the doctors) have never told me I’m cancer-free. They just say there’s no evidence of disease.
“I think medicine and technology are getting better and better and there are a lot of things I could do to help… so I try to think on the bright side.”

