A young mother who had a 5kg cancerous tumor on her ovary growing alongside her baby has revealed how the lesion went unnoticed for so long.
Emily Wiles, 28, from Brisbane, was 33 weeks pregnant with her second child, Eli, when doctors had to perform an emergency caesarean section after finding the huge mass.
Eli, now nine weeks old, spent a short time in the NICU, but was relatively unaffected by the tumor growing alongside him.
While the young woman appears to be safe, Emily has a long road ahead of her and is currently battling through four long months of chemotherapy while caring for baby Eli and her two-year-old little one. Asa with the support of her husband, Luke.
Unfortunately, the tumor was found to be small cell carcinoma of the ovarian hypercalcemic type (SCCOHT), one of the most dangerous types of ovarian cancer.
Emily told FEMAIL that she still doesn’t know what the future holds for her as her type of cancer is rare and very little research has been done to combat it.

Emily Wiles (left) is battling ovarian cancer after a 5kg tumor was discovered in her abdomen when she was 33 weeks pregnant with her son Eli (centre left). Pictured is her with her oldest son Asa (center right) and her husband Luke (right)
“We have a lot of help, which makes a difference, but we’re doing the best we can and trying to spend as much time together as possible,” he said of how they handle the workload.
Emily’s pregnancy with Eli was completely normal until she started experiencing abdominal pain around 30 weeks.
‘That was the only thing that gave anything away. The first few days it was like, ‘Oh, this is a little weird.’ In a way she came and went. Nothing crazy, a little Panadol did it,” she said.
“Every day it got progressively worse. Panadol didn’t help me at all, it was difficult for me to walk and in the end the pain was so much that I couldn’t sleep.’
Despite having a baby, a 5kg tumor and 4kg of fluid growing inside her, Emily’s lump was only slightly larger than normal.
“Everything was pretty normal until later. That photo of me was the morning of the surgery, I would say that’s what my belly looked like when I was almost 40 weeks pregnant with my first,” she said, referring to a Polaroid photo of her in the hospital.
“It was definitely a little bigger, but some people track bigger anyway, so we didn’t think much of it.”
The pain was so unbearable that Emily went to the hospital where she was told it was probably due to problems with her ligaments and that she should see a physiotherapist.
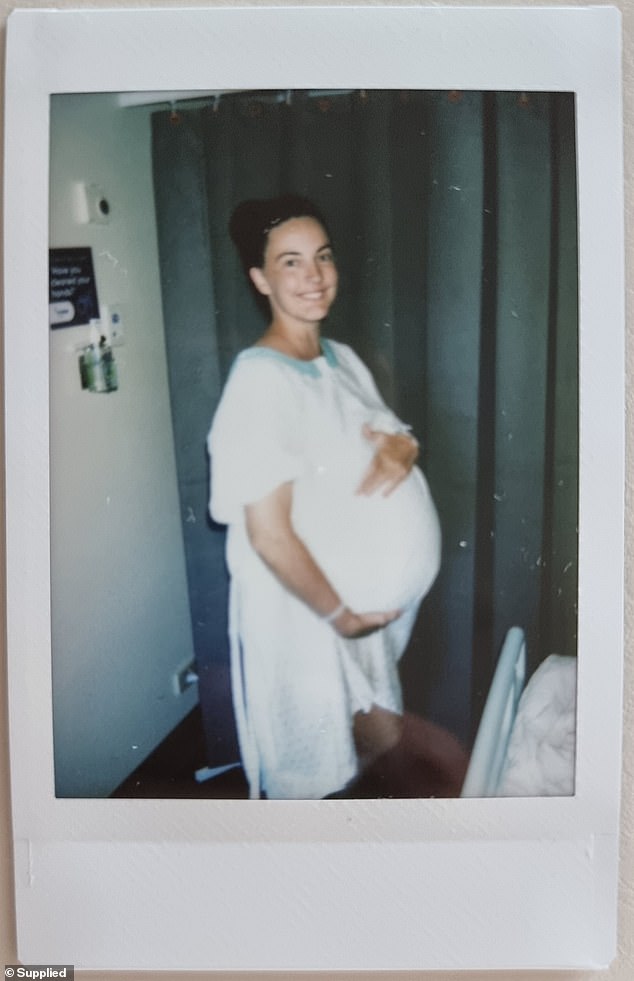
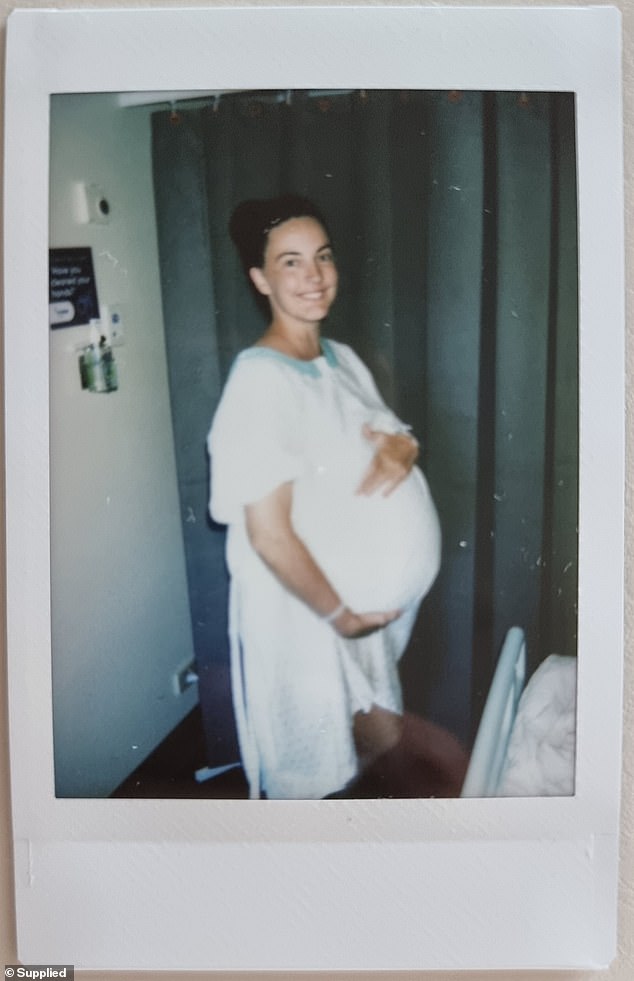
“That photo of me was the morning of the surgery, I’d say that’s what my belly looked like when I was almost 40 weeks pregnant with my first,” Emily said.
“You ask yourself like, ‘Oh, it must just be a pregnancy thing, I need to hold on,’ but it just kept getting worse,” she said.
‘My husband said
“We’re not going to accept if this is going to be the rest of her pregnancy, so we’re going to get another opinion.”
At 31 weeks, she returned to the hospital desperate for answers, where they tested her for a variety of causes, including a urinary tract infection and premature labor, but found nothing.
“I sat there questioning myself trying to figure out how to best manage the pain and they ended up doing an ultrasound after hours,” she said.
‘That’s when (the doctors) discovered there was something there that shouldn’t be. “They didn’t say at the time that they thought it was cancer, I don’t think they really knew.”
The hospital staff told Emily that they had detected something suspicious and that she would have to be transferred to another hospital.
“They said the baby is fine, but something is happening and we need to do more investigations and they just described it as a growth,” she said.


She is undergoing four months of chemotherapy because the tumor was a hypercalcemic type ovarian small cell carcinoma, one of the most dangerous forms of ovarian cancer.
“That’s when we realized this baby was going to be born.”
The next day, Emily had two more ultrasounds and was given the news that the growth was a tumor, but had not yet been determined to be cancerous.
“At that time they were limited to ultrasounds, which don’t really give a complete picture when you look at nothing but the baby,” she said.
“It was quite blurry and difficult for them to determine the size, especially with the baby right next to it. All we knew was that there was something quite big in there and we needed to get it out.
‘It looked like it was going to be some kind of tumor and our reaction was that it was going to be benign because what tumor grows that fast? It is often the benign tumors that grow the fastest.’
The mother was scheduled to have surgery next week to remove the mass and deliver Eli.
Emily was anxious about Eli coming sooner than expected and whether the tumor was going to cause more problems, but she was anxious to stop being in so much pain.


On December 19, 2023, Eli was born by cesarean section seven weeks early and weighed only 2.3 kg. He was taken to the NICU where he recovered uneventfully.
“The pain was completely uncontrollable, even in the hospital with everything they could give me, it was still intense, I can’t even describe it,” he said.
“At first we hoped she would be awake for the delivery, but that was going to be too risky. At that point she had been suffering for so long that she couldn’t wait to operate on me.”
On December 19, 2023, Eli was born by cesarean section seven weeks early and weighed only 2.3 kg.
Mater Mothers’ Hospitals Director of Obstetrics and Gynecology Dr Sarah Janssens, who operated on Emily, said the biggest risk for Eli was being born prematurely, not the tumour.
“Cancer rarely affects the baby or crosses the placenta; the biggest risk to the baby in the womb is the mother becoming unwell,” she explained.
He was taken to the NICU where he recovered without problems.
During surgery, doctors removed a football-sized tumor from Emily’s ovary, as well as 4kg of excess fluid.
“They underestimated the size it ended up being, they definitely didn’t think it was going to be that big,” he said.


During surgery, doctors removed a football-sized tumor from Emily’s ovary, as well as 4kg of excess fluid.
Two days later, while recovering from the procedure, Emily discovered that tests revealed the tumor was ovarian cancer.
“As you can imagine, it was difficult because we had really convinced ourselves, because we wanted it to be that way, that it was benign,” he said.
‘I found it okay, I think what I struggled with was the implications, you have this image of what pregnancy and postpartum will be like. We wanted more kids after Eli, so there were a lot of layers to digest.
“It wasn’t just that I had cancer, but you have cancer, you won’t be able to breastfeed this baby and you’re probably not going to have any more children either, it was a lot to process at once.” .’
Dr Rhett Morton, a gynecological oncologist at Mater Hospital Brisbane, said Emily’s type of cancer, SCCOHT, is a very rare subtype of ovarian cancer and is more likely to affect younger women.
“For every 10,000 women diagnosed with ovarian cancer, no more than one will be diagnosed with SCCOHT,” Dr. Morton said.
Emily started chemotherapy on Christmas Eve, just five days after surgery, and will continue treatment until April.
“Normally they would never do that, have chemotherapy and surgery so close together, but we really had no choice,” he said.
“That was tough and the post-chemo effects of that first round were really tough, especially because I was still recovering from surgery and it really wasn’t very pleasant.”
Dr. Catherine Shannon, senior medical oncologist at Mater Cancer Care Center, said doctors planned to “throw the book” at cancer with chemotherapy and a stem cell transplant.
“The rarity of Emily’s situation makes it very difficult to make an accurate prognosis as there are only a small number of reported cases,” he said.
“The evidence we have suggests that very aggressive treatments provide the best results and survival for the patient, which is why we are considering a stem cell transplant, which will allow us to increase the intensity of the chemotherapy.”
Emily shares her story during Ovarian Cancer Awareness Month to raise awareness of the warning signs of a disease that claims the lives of more than 1,000 Australian women each year.
“If I hadn’t been pregnant, I would have associated the symptoms with periods (cramps, strange bowel movements) and I find that really scary,” she said.
‘I encourage any young person or young women, especially in terms of ovarian cancer, to take their health seriously and if they think something is wrong, to stand up for themselves. Just don’t assume you’ll be fine.
