Health insurance conglomerate UnitedHealth Group is engaged in a secret mission to reduce the company’s costs at the expense of thousands of children with autism, according to an investigation.
Previously undisclosed internal documents obtained by ProPública lay out a plan to limit coverage of the gold standard in therapy for children on the autism spectrum, many of them poor.
Business costs have skyrocketed in recent years along with diagnoses of autism spectrum disorders thanks to increased awareness and better screening tests.
The cost-cutting initiative targets children enrolled through the company’s state-contracted Medicaid plans that serve the nation’s poorest people, including 10,000 children with autism.
The specific therapy targeted by internal documents is applied behavioral analysis, which the company itself admits is the “gold standard, evidence-based treatment for those with medically necessary needs.”
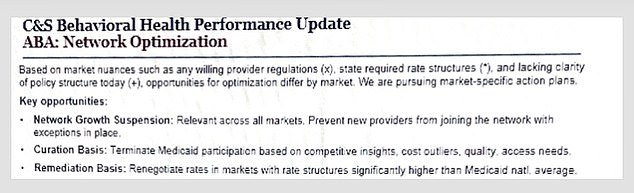
Internal documents show that Optum, which administers mental health benefits for United, aims to “prevent new providers from joining the network” and “terminate” existing ones, even while acknowledging a national shortage of covered counselors.
The company is also organizing “rigorous” clinical reviews to determine the medical necessity of each patient’s therapy, which can lead to coverage denials.
UnitedHealth’s leadership is in hot water over its history of denying medically necessary treatments, an issue that is believed to have led Luigi Mangione, 26, to allegedly murder one of the company’s top executives.
Applied behavior analysis is a very effective form of therapy for children on the autism spectrum that relies on positive reinforcement and repetition. But Optum, the mental health arm of UnitedHealth, is increasingly denying coverage of this “gold standard” therapy across the United States.
UnitedHealth’s mental health division, Optum, aims to limit network expansion and “terminate” existing providers, including those with higher costs, despite long wait times for qualified counselors due to the limited coverage.
Sharelle Menard’s son Benji did not speak for years, having been diagnosed with severe autism when he was three years old.
He was inconsolable as a baby and constantly frustrated because he couldn’t communicate with his mother or anyone else.
But after two years of behavior analysis treatment applied in his home state of Louisiana, the murmurs became little words.
He made great progress with ABA therapy and requires about 33 hours per week to progress.
The disadvantages of insufficient therapy are considerable: from outbursts at school and falling furniture to scratches in the classroom and the inability to learn.
Now, Ms. Menard is worried that Benji will back off after receiving word from Optum that it was refusing to cover the full number of hours her son needs because he had already been in therapy for an extended period but was not making enough progress to graduate. . eventually.
The note from Optum said: ‘Your son is still having a lot of difficulty with all of his autism-related needs. Your son still needs help, but it doesn’t look like he’s going to improve enough to stop ABA.’
ProPublica’s analysis of internal documents found that the company is pursuing “market-specific action plans” to limit children’s access to ABA.
While it was acknowledged that some areas of the country have “very long waiting lists” for ABA therapy, some of the “key opportunities” laid out included “preventing new providers from joining the network,” “terminating” existing providers of the program.
Optum estimated that in some states, provider network cuts could affect more than two-fifths of its in-network ABA therapy groups and up to 19 percent of patients.
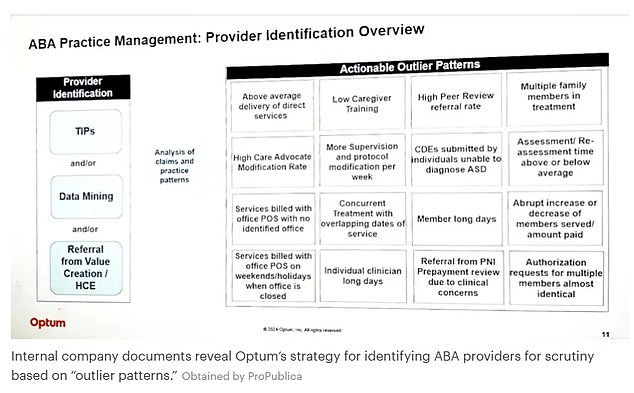
Optum’s internal documents show its strategy for identifying ABA therapy providers that it could justifiably kick out of its network if costs are considered unusually high compared to other providers covered by the network.
Internal documents reveal that Optum has been closely examining ABA providers based on bills and the number of patients they serve.
Aspire and similar providers may be flagged for common patterns in ABA therapy, including billing on weekends or holidays, treating multiple family members in one session, having long medical or patient care hours, providing more services than the average or suddenly increase or decrease the number of patients. or claims.
Optum has repeatedly disputed Aspire’s claims.
Benji had made enormous progress by the time he turned seven. His aggressive tantrums had become less frequent, so it was finally possible to leave the house. He could also pronounce a few dozen words.
Mrs. Menard, a pool cleaner, decided it was time to enroll him in a special education program at school.
But when the insurance company decided not to cover the cost, Benji backed off and reduced his treatment hours.
He swung in gym class, couldn’t sit still, and bit teachers when they tried to discipline him or give him instructions. Over time, his speech also regressed.
Mrs. Menard said, “This motivation and drive… when it’s lost, it’s very difficult to get it back.”
“There’s nothing else that I know of that works.”
She had to withdraw her son from school and enroll him in a home study program run by her therapy group, which costs about $10,000 a year on top of her therapy costs, some of which are still covered by the insurance.
Benji’s doctors wanted to increase his therapy hours from 24 to 33 per week. They hoped the insurer would approve the request since it was less than what had previously been covered and only nine hours more than currently authorized.
But Optum denied the request in May, telling Ms Menard and Benji’s therapists: ‘Your son has been in ABA for six years.
“After six years, more progress would be expected.”

Joslyn McCoy, founder of Aspire, is no stranger to denials of care by Optum. She has continued to provide the necessary hours of therapy to the children even without being reimbursed by the insurance company.

Optum manages mental health benefits for UnitedHealth Group. It is a major driver of company profits; latest estimates put revenue at around $64 billion this quarter.
One of Benji’s therapists and clinical director of the therapy program, Aspire, Whitney Newton, was outraged by the company’s refusal. It was not based on established medical standards for treatment.
She said: ‘We know what you need. It is within our scope of practice and it is our right as a provider to determine it.
“They are cutting and denying an unethical amount.”
By law, health insurers must cover mental health treatments to the same extent as they cover physical illnesses.
A previous ProPublica investigation revealed how United violated the mental health parity law. selectively applying a proprietary algorithm that assesses the medical need for mental health treatments, particularly for ABA.
It was designed to automatically evaluate whether certain therapies were justified based on predefined criteria.
This led to many denials of coverage for therapies deemed “excessive” or “not medically necessary,” even when physicians supported them as essential to the patient’s progress.
Although Optum denied coverage for Benji’s necessary treatment hours, his therapists continued to provide it.
A state administrative judge will decide on an appeal next month for the additional hours Benji needs. If approved, Benji’s therapists will receive payment for six months of services they provided without being reimbursed by the insurance company.
Even if the appeal is successful, the therapists must start over with their dispute with Optum. Each insurance authorization lasts about six months.
Shortly after the hearing date, Benji’s therapists will have to reapply for coverage for his treatment.
Joslyn McCoy, founder of Aspire, said: “We don’t think it’s safe for him to do what the insurance says.”


